Palliative care is becoming an increasingly important part of the spectrum of treatments for patients with cancer, according to David Hui, MD, MSc, of the University of Texas M.D. Anderson Cancer Center in Houston. Dr Hui spoke to science journalists at a recent media briefing on cancer presented by JAMA, the Journal of the American Medical Association.
A fellow in the Department of Palliative Care and Symptom Management at M. D. Anderson, Dr Hui said that cancer is projected to become the number one cause of death worldwide by the end of 2010 and that approximately 1.5 million Americans are diagnosed with cancer annually. Of these patients, 40% have incurable disease, with one-third of deaths occurring within a year of diagnosis.
PALLIATIVE CARE SHOULD BE EARLY CARE
“We know that palliative care is most effective when incorporated early in oncology care,” Dr Hui said. “We’ve recently seen a positive movement among a number of institutions and oncology and patient advocacy organizations pushing for increased palliative care services and early incorporation of such care, but we wanted to better understand how services and programs were structured and what barriers there might be to developing a more consistent approach.”
Dr Hui told the journalists that he and his colleagues at M.D. Anderson and in the Department of Palliative Care at the National Cancer Institute Clinical Cancer Center, Bethesda, Maryland, formulated questionnaires to determine the availability and degree of integration of palliative care services in US cancer centers, as well as to determine their executives’ attitudes toward palliative care. The researchers also sought to compare palliative care services between National Cancer Institute (NCI)-designated cancer centers and non-NCI cancer centers.
SURVEY DETAILS
Questionnaires were sent to 71 NCI-designated cancer centers, as well as to 71 non-NCI cancer centers. The study used two surveys. The first was directed to cancer center executives and requested information regarding access to and attitudes toward palliative care. The second survey was sent only to those cancer centers that had palliative care programs and asked leaders of those programs details about staff, inpatient palliative care units, outpatient clinics, hospice, consultation teams, education, and research.
Some of the survey results are as follows:
· 98% of NCI-designated cancer centers had palliative care programs, but only 78% of non-NCI cancer centers did.
· The NCI-designated cancer centers were better staffed and equipped than the non-NCI cancer centers, with 92% of the NCI centers but only 72% of the non-NCI centers having a palliative care physician on staff.
· 92% of NCI-designated cancer centers had inpatient palliative care consultation teams, compared with 56% of non-NCI centers.
· The study also revealed a large discrepancy in the number of outpatient palliative care clinics, finding that 59% of NCI-designated cancer centers had such clinics while only 22% of non-NCI centers did.
PERCEIVED BARRIERS AND INSUFFICIENCIES
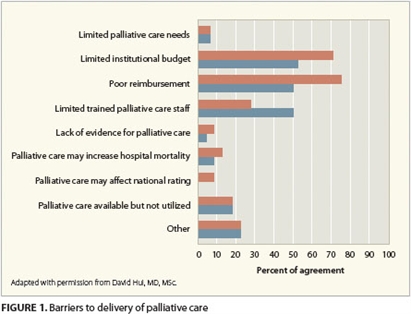 Cancer center executives surveyed said that the most common barriers to their institution’s delivery of palliative care were financial: poor reimbursement and limited institutional resources (Figure 1). Some executives responded that they were concerned that the presence of palliative care could negatively affect their hospital’s mortality rate and national rating. Almost all the cancer center executives agreed, however, that better integration between oncology care and palliative care was desirable.
Cancer center executives surveyed said that the most common barriers to their institution’s delivery of palliative care were financial: poor reimbursement and limited institutional resources (Figure 1). Some executives responded that they were concerned that the presence of palliative care could negatively affect their hospital’s mortality rate and national rating. Almost all the cancer center executives agreed, however, that better integration between oncology care and palliative care was desirable.
More education and research are needed as well. The study found that there are too few palliative care fellowships, research programs, and mandatory rotations for oncology fellows. It also demonstrated that referrals to palliative care are often made later than they should be for the full benefit of the patient and family. The average time from referral to death was 7 days for inpatient consultation teams, 7 days for palliative care units, and 90 days for outpatient clinics.
Dr Hui noted that patient and family referrals to palliative care often took place “too late in their journeys, when the full value of palliative care may not be realized. Much more work remains to be done to improve the quality of care for our patients,” he said.
The study by Dr Hui and colleagues was published in a March 17, 2010 special JAMA issue on cancer (Hui D et al. Availability and integration of palliative care at US cancer centers. JAMA. 2010;303(11):1054-1061). ONA
Bette Kaplan is a medical writer in Tenafly, New Jersey.
