PDF of Cancer Survivorship 0510
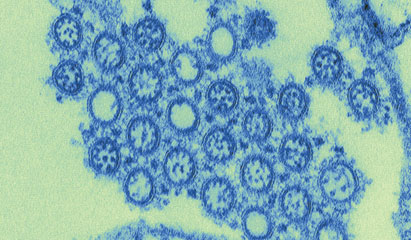
A rigorous program of infection control can avert an influenza outbreak among patients and staff in an immunocompromised population of blood cancer patients, as demonstrated by researchers and medical staff of the Fred Hutchinson Cancer Research Center in Seattle, Washington. Their results are impressive, especially given the 100-fold increase in H1N1 influenza cases in Seattle during the spring of 2009.
There were no increases in the number of H1N1 cases at the Seattle Cancer Care Alliance (SCCA), a facility that concentrates on the screening, diagnosis, and treatment of outpatients who have cancer. The SCCA utilized infection control and vaccination strategies for the patients, their family members, and caregivers. The staff of the facility also benefited from these measures, as what could have been a serious pandemic among clinic patients and staff was quickly identified and controlled.
Corey Casper, MD, Janet Englund, MD, and Michael Boeckh, MD, published a paper about their work in the online version of the journal Blood in December. They wrote, “Lessons learned here are important ones because the majority of cancer care is provided in an outpatient setting. Outpatient cancer care poses more challenges when it comes to protecting patient health because the environment is less controlled than that of a hospital.”1
The infection control program at SCCA was established according to recommendations of the CDC. It is actively used each year from October through April. There are ample hand hygiene stations as well as instructional information about respiratory infections for all patients. In addition, nurses and volunteers administer an 11-point symptom survey to all patients. After completing the survey, each patient receives a sticker, which is color-coded for the day, to signify that he or she has met with the nurse. Patients who have no sticker are denied access to clinical areas.
Outpatients who exhibit symptoms of upper respiratory infection (URI) cannot be seen; they are asked to reschedule appointments and then leave the facility. If they cannot change their appointments, they are given masks to wear and taken to a private room or other isolation area, where they wait to be evaluated by their clinical care team. All of this is documented in patients’ medical records.
 These measures extend to staff as well. The employee sick leave policy is tolerant of absences for respiratory illnesses; any staff member who exhibits symptoms of a URI must stay home until symptoms have resolved. The facility offers respiratory virus testing to those employees who still have minimal symptoms after 4 days at home but who feel well enough to work. They are allowed to work if the test results are negative. There are work plans in case of absences on all staff levels, as well as plans for administering antiviral medication to patients and staff when necessary.
These measures extend to staff as well. The employee sick leave policy is tolerant of absences for respiratory illnesses; any staff member who exhibits symptoms of a URI must stay home until symptoms have resolved. The facility offers respiratory virus testing to those employees who still have minimal symptoms after 4 days at home but who feel well enough to work. They are allowed to work if the test results are negative. There are work plans in case of absences on all staff levels, as well as plans for administering antiviral medication to patients and staff when necessary.
Guidelines for hand hygiene and isolation are strictly adhered to and regularly monitored. All employees must receive an annual influenza vaccination; those who do not must sign a waiver of declination. The authors of this study stress that vaccination is crucial to influenza control, and they strongly urge that facilities where immunocompromised patients are treated require all staff to receive annual influenza vaccinations. Moreover, preventive antiviral therapy should be provided to any unvaccinated staff members who were exposed to confirmed cases of influenza or who were vaccinated less than 3 weeks before being exposed.
The authors conclude, “Our experience shows that aggressive infection control procedures can minimize transmission within the immunocompromised patient population and also reduce acquisition from sources outside the system.” ONA
Bette Kaplan is a medical writer in Tenafly, New Jersey.
Reference
1. Casper C, Englund J, Boeckh M. How we treat influenza in patients with hematologic malignancies [published online ahead of print December 15, 2009]. Blood. DOI:10.1182/blood-2009-11-255455.