The palliative care team is in a unique position to aid patients living with cancer-related fatigue (CRF). Although the problem is widespread and affects patients’ activities of daily living, work, and family life, CRF can often be reversed or at least alleviated with a number of interventions. The most important step in alleviating CRF is to establish its cause.
IS ANEMIA TO BLAME?
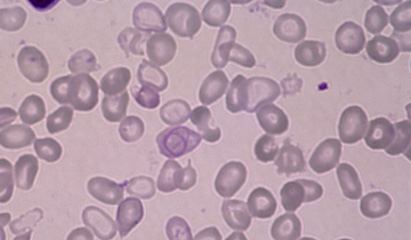
A common cause of fatigue, asthenia, and weakness among patients coping with cancer, anemia may be a result of the disease itself or its treatment with chemotherapy or radiation. Anemia is often reversible. An approach as simple as iron supplementation may help, but in more severe cases, an erythropoiesis-stimulating agent (ESA) is needed. When epoetin alfa (Epogen, Procrit) or darbepoetin alfa (Aranesp) is administered to raise hemoglobin (Hb) levels, medical staffers note a positive correlation between patients’ physical and psychological improvement and their Hb levels.
The American Society of Clinical Oncology (ASCO) and the American Society of Hematology (ASH) recommend administering an ESA when Hb approaches or reaches 10 g/dL, both to increase Hb and to decrease transfusions.1 The 2007 ASCO/ASH clinical practice guideline update provides information that addresses giving ESAs to patients who are at risk for thromboembolic complications.1
SLEEP PLAYS A ROLE
As with fatigue, sleep disturbance is also associated with cancer and cancer treatment. The sleep problem causes further fatigue, and the two affect the patient’s functioning. Since the sleep problem and fatigue occur together, some cancer researchers suggest that a reciprocal relationship may exist between the two. Although in some patients, pharmacologic intervention for insomnia may not be effective by itself, several studies have demonstrated the benefit of cognitive behavior therapy for insomnia (CBT-I) in conjunction with pharmaceutical agents. According to one review of the role of sleep in CRF, “treating clinically significant insomnia is likely to have benefits for the patient with cancer and for those who are recovering from cancer. In particular, pharmacotherapies for insomnia, singly or in combination with CBT-I, should be evaluated in [multicenter] randomized clinical trials to examine their efficacy in improving sleep quality and reducing associated CRF.”2
EXERCISE: INCREASINGLY IMPORTANT
Exercise is beneficial for most people, and cancer patients dealing with fatigue are no exception. Many studies cite the importance of supervised exercise programs in palliative care. The notion that moving about can actually alleviate fatigue may appear paradoxical, but exercise helps people sleep better so they feel less tired and less depressed. In fact, patients who exercise on a regular basis can reduce their CRF by up to 50%. Furthermore, exercise increases muscle mass and flexibility. The better a patient’s physical condition, the more successful that person is at coping with surgery and other cancer treatments. An exercise program elevates mood, promotes weight normalization, and improves cardiovascular conditioning—all essential factors for cancer survivorship.
In a recent paper published online in the British Medical Journal, a supervised exercise program significantly improved fatigue in cancer patients undergoing chemotherapy.3 In another study, palliative care nurses observed, “Only exercise had a significant direct effect on fatigue.”4 Those practitioners, in Incheon, Korea, have developed a structural model of the factors affecting CRF. Their goal is to help oncology nurses understand the syndrome and be able to evaluate and correct CRF symptoms in patients. Their model comprises a number of entities: physical and psychological distress, as well as sleep-related, physiologic, physical performance, and exercise factors.
In March 2010 at the 16th International Conference on Cancer Nursing in Atlanta, Georgia, Jennifer Wenzel, PhD, RN, of the Johns Hopkins School of Nursing in Baltimore, Maryland, presented the results of a randomized trial evaluating an exercise intervention among patients with cancer. According to the study findings, patients who were prescribed exercise while being treated for cancer had less emotional distress, less fatigue, and more vigor than did the less active patients in the trial.5
COUNSELING AND OTHER TECHNIQUES
Palliative care teams find that counseling and education are beneficial for patients experiencing CRF. As part of this process, they evaluate the patient’s level of fatigue and discuss the reasons for the symptoms. Patient and practitioner then talk about the available treatments and interventions. In addition to covering the treatment of anemia and sleep disturbance, team members review such topics as incorporating exercise in the patient’s day while ensuring that the patient gets enough rest.
Some palliative care teams include a massage therapist. Others ensure that yoga or relaxation techniques are available to patients. Nutritionists also play a role in alleviating CRF since many patients with cancer do not, or cannot, meet their nutritional needs and suffer the debilitating consequences.
In a recently published study of fatigued breast cancer survivors, researchers suggest that patients with cancer could benefit from receiving early intervention, even prophylaxis, for such common symptoms as depression and sleep disturbance. They write that the fatigue of cancer may be a coping mechanism, requiring the patient to get more rest and conserve energy, expending it only on those activities that are important.6 ONA
Bette Kaplan is a medical writer in Tenafly, New Jersey.
References
1. Rizzo JD, Somerfield MR, Hagerty KL, et al. Use of epoetin and darbepoetin in patients with cancer: 2007 American Society of Clinical Oncology/American Society of Hematology clinical practice guideline update. J Clin Oncol. 2008;26(1):132-149.
2. Zee P, Ancoli-Israel S; Workshop Participants. Does effective management of sleep disorders reduce cancer-related fatigue? Drugs. 2009;69 suppl 2:29-41.
3. Adamsen L, Quist M, Andersen C, et al. Effect of a multimodal high intensity exercise intervention in cancer patients undergoing chemotherapy: randomised controlled trial. BMJ. 2009;339:b3410. http://www.bmj.com/cgi/content/full/339/oct13_1/b3410?view=long&pmid=19826172. Accessed May 5, 2010. doi:10.1136/bmj.b3410.
4. Seo Y, Oh H, Seo W. Causal relationships among factors associated with cancer-related fatigue [published online ahead of print November 26, 2009]. Eur J Oncol Nurs. doi:10.1016/j.ejon.2009.09.008.
5. Wenzel J, Griffith K, Shang J, et al. Results of a home-based walking intervention for patients undergoing cancer treatment. Paper presented at: 16th International Conference on Cancer Nursing (ICCN); March 7-11, 2010; Atlanta, GA. Abstract O-36.
6. Banthia R, Malcarne VL, Ko CM, et al. Fatigued breast cancer survivors: the role of sleep quality, depressed mood, stage and age. Psychol Health. 2009;24(8):965-980.