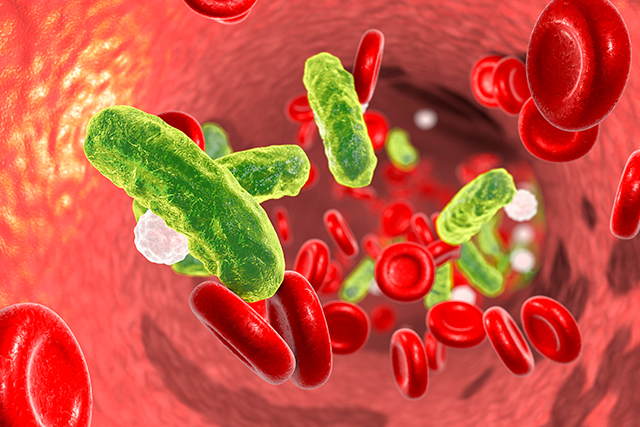
Sepsis and septic shock are life-threatening conditions triggered by dysregulated immune reactions to infection.1 Clinical vigilance as well as timely diagnosis and treatment are crucial to patient survival.
Neutropenic sepsis and septic shock are common oncologic emergencies, and patients face higher risks of death from cancer-related sepsis hospitalizations than from other sepsis hospitalizations.1 More than 20% of sepsis hospitalizations in the United States are cancer-related cases, according to an analysis of more than 1 million sepsis patients.2 Fever is frequently the only sign of neutropenic sepsis in patients with cancer, but not all patients develop fever.1 Radiotherapy and systemic chemotherapy-associated sepsis (along with pneumonia and acute kidney injury) are leading causes of emergency department admissions among cancer patients.3
The exact magnitude of the global burden of sepsis and septic shock remains unclear in part because of varied definitions and clinical criteria used in their diagnosis.1 But sepsis and septic shock are recognized as leading causes of death, and 6 million to 11 million people are believed to die from these conditions each year, accounting for up to 20% of all deaths worldwide.1,4 The World Health Organization declared sepsis a global health care priority in 2017.4 In the United States, an estimated 33% to 50% of all in-hospital deaths are associated with sepsis.1
Sepsis is defined by the Society of Critical Care Medicine and the European Society of Intensive Care Medicine as a life-threatening organ dysfunction arising from inflammation and other immune reactions to infection. Septic shock involves metabolic- and vasodilation-associated vascular and circulatory dysfunction that further increase patients’ risk of death.5,6 Systemic vasodilation and microvascular dysfunction disrupt blood flow to vital organs.1
Risk Factors
Oncology nurses need to be able to recognize which of their patients with cancer may have an increased risk of developing sepsis. Demographic and lifestyle risk factors for sepsis overlap with those of cancer and include obesity, age older than 65 years, income level, tobacco use, dental carries (cavities), and low levels of exercise.1,7 Regional variation in sepsis incidence and outcomes have been noted; a “sepsis belt” in the southeastern United States appears to be driven by patterns of patient income, tobacco use, and comorbidities such as diabetes and chronic obstructive pulmonary disease.1,8
In addition, patients with depression, anxiety, or substance abuse face an increased risk of developing sepsis.1
Clinical risk factors include immunosuppressive medications and therapies such as radiotherapy, chemotherapy, immunotherapy, cellular therapies, and steroids, as well as previous hospitalizations (possibly reflecting in part microbiome changes associated with antibiotic administration during inpatient treatment).1 Cancer survivors also face elevated sepsis risk, so a previous cancer diagnosis should be considered a risk factor.1
Patients with acute leukemias, advanced tumor stage, and delays in admission to a hospital or an intensive care unit (ICU) are more likely to develop bacteremia, sepsis, and septic shock. Up to 30% of patients with neutropenic cancer who are on a cytotoxic chemotherapeutic regimen will develop sepsis, but the incidence rates associated with external beam radiotherapy for most cancer types are unknown.1 Nineteen percent of patients undergoing chemoradiation for head and neck cancer develop infections, and resulting sepsis underlies most deaths within 30 days of concluding treatment.9,10
Another important risk factor of radiotherapy- and systemic chemotherapy-associated bloodstream infection (bacteremia), sepsis, and sepsis shock is intestinal mucositis (disruption of the mucosal lining).9 Proinflammatory cytokines and the release of matrix metalloproteinase and other enzymes trigger cellular and tissue death.9 Resulting ulcerations allow gut bacteria to escape from the intestinal tract, causing bacteremia and sepsis.9 Mucositis also contributes to an increased risk of bacteremia in patients undergoing hematopoietic stem cell transplantation.9