Three-dimensional (3-D) conformal intensity-modulated radiotherapy (IMRT) has become widely available across the United States over the past decade. Despite a relatively small empirical literature regarding this modality’s indications and efficacy and its relatively complex treatment planning and implementation process, IMRT is becoming an increasingly routine treatment for brain, head and neck, colorectal, and prostate cancers. Studies suggest that IMRT may offer patients reduced GI toxicities compared with conventional radiotherapy, but evidence of efficacy is weak. Driven partly by reimbursement incentives, however, IMRT has become a controversial first-line treatment for prostate cancer. Critics warn that it is an inappropriate treatment for many patients and that adoption of IMRT by a cancer center requires careful staff training to avoid dosing errors and suboptimal treatment.
PROSTATE CANCER AND THE RADIOTHERAPY DILEMMA
Last year, prostate cancer was diagnosed in an estimated 217,700 US men, and more than 30,000 died of this malignancy, according to the National Cancer Institute (NCI).1 Treatment options include surgical removal of the prostate, brachytherapy with radiation pellets placed around the tumor, external beam radiotherapy, chemotherapy, and combinations of these modalities. Surveillance and monitoring of tumor progression is also an option, particularly for men older than 80 years, among whom prostate cancer frequently is a smaller threat to survival than other diseases and medical events.
In older patients, treatment can significantly impair quality of life, and recovery from treatment can be slow. Moreover, treatment complications and side effects are common. Prostate resection is associated with sexual impotence and urinary incontinence, for example, and irradiation can cause rectal bleeding.
 External beam radiation is a frequent component of prostate cancer treatment. As with all radiation therapies, however, this treatment involves the fundamental dilemma of how to deliver therapeutic (ie, cell killing) doses of radiation to tumor tissue while minimizing irradiation of healthy tissue adjacent to tumors or situated along external radiation beam pathways. Universal tumor control could be achieved except for this trade-off.
External beam radiation is a frequent component of prostate cancer treatment. As with all radiation therapies, however, this treatment involves the fundamental dilemma of how to deliver therapeutic (ie, cell killing) doses of radiation to tumor tissue while minimizing irradiation of healthy tissue adjacent to tumors or situated along external radiation beam pathways. Universal tumor control could be achieved except for this trade-off.
One solution to the dilemma is fractionation, or division of the total therapeutic dose of radiation to be delivered, over a series of irradiation sessions. Fractionation minimizes irradiation of nontarget tissue and allows time for healthy, incidentally irradiated tissue to recover between treatment sessions. However, tumor radioresistance can evolve quickly when sublethal dose fractions are delivered to tumor tissue, and radioresistance remains a leading cause of radiotherapeutic failure.
INTENSITY-MODULATED RADIOTHERAPY
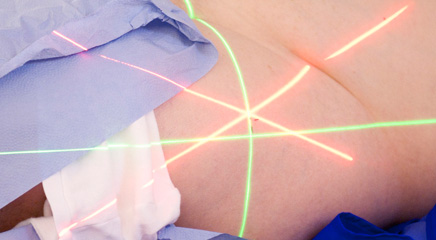
IMRT, an advanced and more precise external beam radiotherapy introduced in the 1990s, allows another solution to the radiotherapy dilemma: The intensity of the radiation beam is modulated through selective contouring of multiple beam pathways delivered from different directions to maximize tumor radiation doses while minimizing irradiation of healthy tissues along any given beam pathway. Treatment planning is complex, based on 3-D CT imaging and use of computer dosimetric algorithms to calculate the best series of beam pathways for irradiating tumors with irregularly shaped volumes. This approach provides higher cumulative radiation doses to target tissues than can safely be achieved with conventional external beam radiotherapy. CT images obtained between radiation sessions allow recalibration of sculpted irradiation as tumor volume decreases and tumor contours change with treatment. Compared with other radiation modalities, IMRT permits more precise irradiation of concave tumors, including those enveloping nontarget tissues, such as vasculature or the spinal cord.
Assuming that 3-D CT imaging is of sufficiently high quality, IMRT should make possible precise delivery of radiation along complex tumor contours, minimizing the need for therapeutic margins (volumes of healthy tissue around a tumor that are irradiated to kill undetected tumor cells near the target tumor). Although IMRT requires longer treatment sessions and exposes greater total volumes of healthy tissue to low-dose radiation, this treatment modality should allow safe delivery of escalated irradiation of tumors; better local tumor control; and ultimately, longer patient survival, with reduced harm to healthy tissues and resulting toxicities.
THE ROLE OF IMRT IN PROSTATE CANCER
Intensity-modulated radiotherapy is the standard of care for head and neck cancers, and it shows great promise for the treatment of certain brain and colorectal cancers. More controversially, however, IMRT at some cancer centers has also become a de facto standard of care for prostate cancers.
A recent systematic review of data from 13 studies representing 5,768 patients suggests that IMRT may be appropriate for patients with moderate- or high-grade prostate tumors because it appears to spare rectal tissue from unnecessary irradiation. The result would be fewer GI complications, such as rectal bleeding, pain, and uncontrolled defecation.2 However, reported complications varied between studies, with some studies in the review suggesting that IMRT may increase urinary incontinence and urinary tract bleeding.2 A separate 2008 systematic review that examined prostate cancer data from 16 studies also found reduced toxicity with IMRT but noted that evidence for local tumor control and overall patient survival were generally inconclusive.3 “Significantly decreased gastrointestinal or genitourinary toxic effects were reported for the IMRT groups,” the authors of the 2008 study reported.3 Despite the promise that IMRT may hold for high-risk prostate cancer patients, critics like American Society for Radiation Oncology chairman Anthony Zietman have cautioned that IMRT is likely being overprescribed for other patients in whom this approach is suboptimal.
Use of IMRT is partly driven by financial incentives, critics believe.4 Hospitals and academic cancer centers tend to use IMRT primarily for complex head and neck cancers and for lung cancers, but Medicare pays up to $40,000 per patient for any IMRT prescribed, whether treatment is for a complex head and neck cancer or a relatively simple prostate tumor, Zietman says. Brachytherapy or even active surveillance may frequently offer better solutions for patients, but disproportionate reimbursements represent a powerful financial incentive to use IMRT as a first-line treatment for prostate cancer. “Urologists appear to frequently diagnose prostate cancers and channel patients to IMRT without presenting other choices,” Zietman said. “It is unlikely they are presenting the no-treatment option. That narrowing of [patient] choice disturbs me.”
In areas where private IMRT urology clinics have been established, local rates of brachytherapy and prostatectomy have declined sharply, Zietman and others note. Elderly patients who should be left alone are receiving IMRT at many clinics, Zietman adds. Given the potential impacts that radiotherapy can have on patients’ quality of life, the practice is not justified, critics charge. “It is almost elder abuse,” Zietman said. “There is zero evidence of benefit” for IMRT in elderly men. Unfortunately, no guidelines yet exist on the indications for IMRT in patients with prostate cancer.
Also to be considered is that IMRT is inherently more complex than other therapies. This modality requires intensive training of staff and constant surveillance of quality control to avoid radiation dosing errors and suboptimal dose distributions, some have cautioned.5 ONA
Bryant Furlow is a medical writer based in Albuquerque, New Mexico.
REFERENCES
1. National Cancer Institute. Estimated new cancer cases and deaths for 2010. http://seer.cancer.gov/csr/1975_2007/results_single/sect_01_table.01.pdf. Accessed March 22, 2011.
2. Hummel S, Simpson EL, Hemingway P, et al. Intensity-modulated radiotherapy for the treatment of prostate cancer: a systematic review and economic evaluation. Health Technol Assess. 2010;14(47):1-108.
3. Veldeman L, Madani I, Hulstaert F, et al. Evidence behind use of intensity-modulated radiotherapy: a systematic review of comparative clinical studies. Lancet Oncol. 2008; 9(4):367-375.
4. Furlow B. US urology clinics overprescribe prostate radiotherapy. Lancet Oncol. 2011; 12(2):122.
5. MacKay RI, Staffurth J, Poynter A, et al. UK guidelines for the safe delivery of intensity-modulated radiotherapy. Clin Oncol (R Coll Radiol). 2010;22(8):629-635.