| The following article features coverage from the 2018 Oncology Nurse Advisor Navigation Summit. Click here to read more news highlights and expert perspective from the Summit on Oncology Nurse Advisor. |
Immunotherapy is a novel, rapidly evolving cancer treatment with exciting benefits but also unique challenges for patients and their health care team. Navigation is a pivotal component in the care of patients undergoing treatment with these therapeutic agents, Kelly J. Brassil, PhD, RN, AOCNS®, ACNS-BC, explained in a presentation at the 2018 Oncology Nurse Advisor (ONA) Navigation Summit.
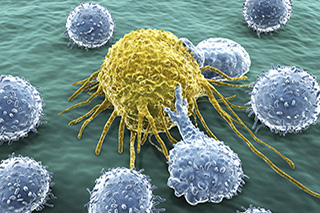
Immunotherapeutic agents are used to maximize the immune system’s innate response. These agents have the power to regress and eliminate cancer growth using the body’s own immune system. Having been in development for more than a century, immunotherapy was first tested by injecting streptococcal organisms into a patient with an inoperable sarcoma that led to regression of cancer growth.
Immunotherapies are generally classified as 4 classes of agents: Monoclonal antibodiesbind to and block signaling pathways on the surface of cells leading to inhibition of proliferation, activation of apoptosis, and re-sensitization of malignant cells to cytotoxic agents. Checkpoint inhibitorsare defined as agents that take the brakes off the immune system, releasing a series of pathways in the immune system that regulate the activation of T-cells. Immune effector cellsare a cellular treatment that involves therapeutically reprogramming T-cells to target tumors, specifically CD19 antigen — which is highly expressed in B-cell malignancies — and CD24 antigen. Oncolytic viral therapiesuse viruses — both nonpathogenic (harmless to humans) and pathogenic (requires genetic modification for use) — to induce apoptosis among malignant cells.
These treatment options offer significant benefits, including remarkable tumor response in diverse malignancies, potential to be a curative treatment, fewer standard toxicities than what is observed with chemotherapy or radiotherapy, and the potential to produce an enduring immune response. But with the benefits are challenges: Unique toxicities of these treatments can be fatal. Immunotherapy is not proven effective in some tumor types, nor is it effective for some patients. It has a high cost — sometimes in excess of $300,000, and that is just for the drug not including the other care needed, Dr Brassil pointed out.
An excessive release of cytokines, often a result of T-cell activation, is the cause of many immunotherapy-related adverse effects (irAEs). This release causes inflammation to both healthy and cancerous surrounding tissues. Neurotoxicity, an irAE of the immune effector cell therapy chimeric antigen receptor (CAR)-T cell therapy, can be fatal. Because irAEs are often inflammatory in nature, primary management is steroids.
Immunotherapy and its adverse effects are distinct from other types of cancer treatment, therefore, nurses and patients need to understand that immunotherapy is not chemotherapy. Its adverse effects require early identification and unique management to prevent potentially terminal progression, Dr Brassil stressed. For this reason, navigation is an essential part of using immunotherapy.
Because many immunotherapeutic agents are administered in the ambulatory setting, patients need care coordination for follow-up in case acute toxicity occurs. CAR T-cell therapy is administered in only 32 sites, but patients are sent back to their local communities for follow-up and further care. Navigators need to be prepared to direct care for these patients when they return to their home care environment. These patients may experience long term sequelae that need immediate and unique management, and need continued support throughout their care to optimize outcomes.
Key considerations that navigators can help patients understand: Immunotherapy does not work for everybody. Its costs can be significant and insurance approval may be challenging. Many patients were treated on clinical trials, so financial factors may not have been as significant. Patients who received immunotherapy may experience late effects, such as long-term immunogenicity. How this affects future malignancies or even infections is not yet known. Immunotherapies may be used alone or in combination with other immunotherapy agents or types of cancer treatments.
Support resources for patients and their navigators include immunotherapy pocket cards; toxicity guidelines from ASCO/NCCN (published in February), SITC, and ESMO; and immunotherapy education from ONS. However, Dr Brassil cautions that research and clinical trials with these therapies are ongoing and what is known today is very likely to change tomorrow.
Reference
Brassil KJ. Navigating patients receiving immune-oncology treatment. Oral presentation at: 2018 ONA Navigation Summit; June 14-16, 2018; Chicago, IL.