Metastatic bone tumors are a major cause of suffering and functional impairment for patients with cancer, degrading quality of life. They also represent the single most frequent cause of pain encountered in clinical oncology.1 Bone metastases can also cause debilitating complications such as spinal cord compression, pathogenic bone fractures, and hypercalcemia.2
Palliative radiotherapy plays a central role in treating pain caused by skeletal metastases. In US clinical practice, palliative radiotherapy doses and fractionation schedules vary from center to center; however, results of several prospective clinical trials suggest single-fraction radiotherapy is as effective as prolonged, multi-fraction palliation regimens.1,2
In early 2011, the American Society for Therapeutic Radiology and Oncology (ASTRO) released new evidence-based treatment guidelines for radiotherapeutic palliation of bone metastases, based on a comprehensive task force review of published studies.2 The new ASTRO guidelines call for changes in patterns of care for patients with bone metastases.
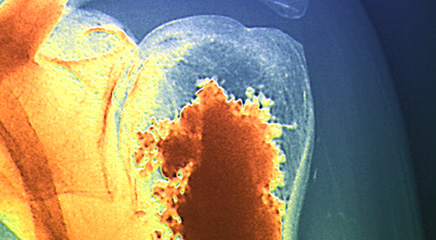
SKELETAL METASTASES
Metastatic skeletal tumors are common. Up to 80% of patients with prostate cancer and breast cancer and up to 40% of patients with thyroid carcinoma, lung cancer, and renal cell carcinoma develop bone metastases.1,3-4Patient prognosis varies dramatically, depending on the cancer type involved; lung cancer patients with bone metastases rarely survive 6 months, but prostate and breast cancer patients, properly treated, may survive for 3 years or more.1 The 5-year survival rate for prostate cancer patients with bone metastases is 25% and the median survival time is 40 months.3
Skeletal metastases are described as bone-destroying (osteolytic), bone-growing (osteoblastic), or both (mixed).1These tumors may be uncomplicated or involve pathogenic fractures or spinal compression.1 Radiation kills tumor cells and inhibits bone destruction caused by secretion of osteoclast activating factors (OAFs), reducing the risk and progression of fractures and compression.2
 Treatment options for painful bone metastases include bisphosphonates (for osteoblastic or mixed-type tumors); radiotherapy; and for pathogenic fractures, corticosteroids, surgery, kypho plasty, or vertebroplasty.1,2 External beam radiotherapy (EBRT) is the current gold standard and most frequent treatment modality for pain stemming from bone metastases.2 Less conclusive clinical data suggest stereotactic body radiotherapy (SBRT) may also be a useful modality for some patients with spinal metastases.2 EBRT palliation of asymptomatic (nonpain inducing) bone metastases has been criticized by some authors as not useful.5
Treatment options for painful bone metastases include bisphosphonates (for osteoblastic or mixed-type tumors); radiotherapy; and for pathogenic fractures, corticosteroids, surgery, kypho plasty, or vertebroplasty.1,2 External beam radiotherapy (EBRT) is the current gold standard and most frequent treatment modality for pain stemming from bone metastases.2 Less conclusive clinical data suggest stereotactic body radiotherapy (SBRT) may also be a useful modality for some patients with spinal metastases.2 EBRT palliation of asymptomatic (nonpain inducing) bone metastases has been criticized by some authors as not useful.5
THE NEW GUIDELINES
ASTRO released new treatment guidelines for palliative radiotherapy of painful bone metastases in February 2011. The guidelines are based on a systematic review of 25 randomized trials, 20 prospective single-arm studies, and four meta-analyses conducted by ASTRO’s 17-member expert task force.2
EBRT is the mainstay for treating uncomplicated skeletal metastasis pain, and palliation can be safely and effectively delivered with a single EBRT fraction of 8 Gy, the ASTRO task force concluded.2 Follow-up retreatment with single-fraction 8 Gy is also safe and effective, with comparable risks of side effects.2 “Although various fractionation schemes may provide good rates of palliation, numerous prospective randomized trials have shown a single 8 Gy fraction to provide noninferior pain control and side effect risks compared to longer fractionation schemes,” the ASTRO guidelines state.2
Pain relief benefits associated with the single-fraction regimen are comparable to those achieved with multi-fraction regimens: 50% to 85%, with variation reflecting differences between trials in how pain and pain relief were assessed.2 Multifraction regimens may frequently be unnecessary and, given the expense and time requirements for patients and staff, unjustified in many cases.2 However, multifraction EBRT may have useful benefits for patients with favorable prognoses and relatively long life expectancies.1 For example, multifraction EBRT is associated with significantly superior remineralization of osteolytic tumor-degraded bone—an important factor in the treatment of pathogenic bone fractures.1 Multifraction regimens also yield fewer cases of recurrent spinal compression.1
A recent survey, cited in the ASTRO guidelines, suggests that despite these published trial data significantly fewer US radiation oncologists prescribe a single-fraction palliative radiotherapy regimen compared with oncologists in Europe and elsewhere. This reflects a delay in the incorporation of evidence into US clinical practice.2,6 The ASTRO task force called for a change in patterns of practice, with more widespread adoption of single-fraction palliation.2
Radionuclides may be a useful palliative modality for patients with multiple painful osteoblastic foci.2Bisphosphonates or radionuclides, however, should not be considered an alternative to EBRT.2 Indeed, bisphosphonates, which are indicated in cases of osteoblastic or mixed bone metastases, appear to slow osteoclast activity.2 No phase III clinical trials have compared EBRT alone with EBRT plus bisphos phonates, suggesting that bisphospho nates may function synergistically with EBRT, which inhibits OAF production in tumors.2
“EBRT and bisphosphonates have a theoretic ability to act in a complementary fashion because of their local versus systemic spatial cooperation and also because their toxicity profiles do not significantly overlap,” the ASTRO guidelines state.2 “Bisphosphonates appear safe and effective when combined with either single or multiple fraction radiotherapy (although) the Task Force could not find data to recommend one bisphosphonate or fractionation scheme in combination as having greater efficacy than another.”2
SPINAL METASTASES
As many as 40% of cancer patients will experience spinal metastases, but fewer than 3% will suffer spinal cord compression-related functional or sensory impairments or incontinence.2 Surgical decompression should be discussed and coordinated with a neurosurgeon and radiation oncologist, and only undertaken when patients are good surgical candidates and have relatively long life expectancies.2 When kyphoplasty and vertebroplasty (percutaneous injection of bone cement to fracture sites to stabilize bone and reduce pain) are indicated, treatment should be in conjunction with EBRT, not as an alternative to EBRT.2
Although empirical evidence for optimal postsurgical EBRT dosing is inconclusive, most facilities utilize multiple-fraction regimens, such as 30 Gy in 10 fractions, to kill micrometastases.2 Studies of single-fraction palliative EBRT after spinal decompression surgery have not been published; however, patients who are not candidates for surgery may benefit from improved progression-free survival and local control as well as improved pain control from EBRT alone.2
MORE EVIDENCE NEEDED
SBRT holds theoretical promise for patients with spinal metastases because it can deliver high radiation doses to target metastases in the spine while sparing adjacent nerve tissues in the spinal cord and cauda equina, concluded the ASTRO task force.2 However, because published studies consist largely of single-institution retrospective reviews and SBRT dosing and targeting standards are not yet fully defined, SBRT should be used only in carefully selected cases as part of a prospective clinical trial and used only at high-volume treatment centers that have experience with SBRT dosimetry and risks.2 ONA
Bryant Furlow is a medical writer based in Albuquerque, New Mexico.
REFERENCES
1. Rades D, Schild SE, Abrahm JL. Treatment of painful bone mestastases. Nat Rev Clin Oncol. 2010;7(4):220-229.
2. Lutz S, Berk L, Chang E, et al. Palliative radiotherapy for bone metastases: an ASTRO evidence-based guideline. http://www.astro.org/Research/CommentForm/documents/BoneGLDraft.pdf. Accessed September 19, 2011.
3. Sturge J, Caley MP, Waxman J. Bone metastasis in prostate cancer: emerging therapeutic strategies. Nat Rev Clin Oncol. 2011;8(6):357-368.
4. Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res. 2006;12(20 Pt 2):6243s-6249s.
5. Lutz S, Korytko T, Nguyen J, et al. Palliative radiotherapy: when is it worth it and when is it not? Cancer J. 2010;16(5):473-482.
6. Fairchild A, Barnes E, Ghosh S, et al. International patterns of practice in palliative radiotherapy for painful bone metastases: evidence-based practice? Int J Radiat Oncol Biol Phys. 2009;75(5):1501-1510.