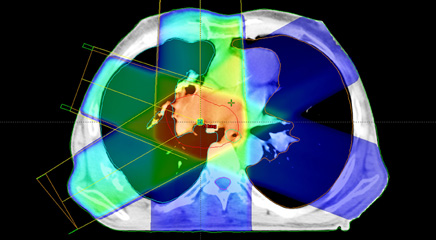
Nearly two-thirds of cancer patients receive radiation therapy. However, irradiation of healthy, nonmalignant tissue around the tumor and along the radiation beam pathway can cause morbidity and increases the risk of secondary cancers, particularly in younger patients, limiting therapeutic radiation doses that can be delivered to the tumor.
Advances in robotic positioning, computers, and real-time imaging are improving radiotherapy planning, fractionation, and the precision of radiation delivery, reducing target margins to allow more aggressive stereotactic radiotherapy regimens and improved tumor control—even in challenging cancers with complex tumor contours, according to speakers at the Future of Radiation Medicine 2011 symposium.1,2 The symposium was held in Scottsdale, Arizona, February 17, and was sponsored by Elekta Oncology (Stockholm, Sweden; www.elekta.com), which produces stereotactic radiotherapy systems and other radiation therapy equipment and information systems. Speakers at the symposium have received research support from Elekta.
Presentations described emerging radiotherapy modalities for breast, lung, and liver cancer; metastatic brain cancer; and complex spine tumors, and research into the supplementation chemotherapy regimens that target molecular pathways in patients with some genetic cancer risks with these radiotherapy modalities. Summary papers and video presentations from the symposium are available online.1,2 Researchers at the symposium also discussed the promise of emerging radiotherapy techniques for managing chronic pain and neurodegenerative disorders.
Cancer radiotherapy outcomes have been blatantly unsatisfactory for patients, according to Professor of Radiation Oncology and Neurosurgery Robert D. Timmerman, MD (University of Texas Southwestern, Dallas); although, patient-reported outcomes are rarely the end point focus of clinical trials. “In the future, radiation therapy for cancer will be significantly different than today’s treatments, simply because current outcomes are unsatisfactory to patients,” Timmerman said at the symposium.
 Large prospective radiotherapy patient registries that track survival, disease recurrence, and quality of life are needed to facilitate comparative effectiveness research on patient outcomes, Timmerman said. He supports the American Society for Radiation Oncology (ASTRO)’s proposal for a national clearinghouse for all clinical cancer treatment study data to ensure that researchers have access to both positive and negative trial data, with which truly evidence-based standards can be developed.
Large prospective radiotherapy patient registries that track survival, disease recurrence, and quality of life are needed to facilitate comparative effectiveness research on patient outcomes, Timmerman said. He supports the American Society for Radiation Oncology (ASTRO)’s proposal for a national clearinghouse for all clinical cancer treatment study data to ensure that researchers have access to both positive and negative trial data, with which truly evidence-based standards can be developed.
AN EMERGING STANDARD OF CARE
Just as computerized treatment planning, multileaf collimators and intensity-modulated radiotherapy (IMRT), and 3-dimensional conformal radiotherapy improved precision and reduced the severity of morbidity throughout the 1990s, Timmerman predicted, technological advances are allowing image-guided hypofractionated stereotactic body radiation therapy (SBRT; also known as stereotactic ablative radiotherapy [SABR]) to emerge as a standard of care for lung, liver, and spine tumors in patients who are not candidates for surgery.3,4
Increased radiation targeted allows delivery of larger fractions of optimal therapeutic radiation doses at each patient visit, thereby reducing the overall time of therapy. Conventional external-beam radiotherapy will be supplanted by SBRT or image-guided hypofractionated radiotherapy (IGHRT), which he described as a hybrid between SBRT and conventional radiotherapy. IGHRT offers real-time imaging to track and accommodate tumor motion, such as that caused by patient respiration—a major challenge in hypofractionated lung tumor radiotherapy—and allows so-called 4-dimensional conformal irradiation of tumor tissue. IGHRT is already widely used for breast and prostate cancer. Clinical research of SBRT for the treatment of metastatic bone and lymph node tumors, and primary breast, prostate, pancreas, and kidney cancer is now underway.3
Radiation oncologist Brian D. Kavanagh, MD (University of Colorado at Denver), who has collaborated with Timmerman, also sees a central role for IGHRT or SBRT for cancer radiotherapy within the coming decade. “It’s very possible that within 10 years a huge percentage of patients—particularly those with prostate, breast, and lung cancers—will be treated completely, even with a curative intent, with IGHRT or SBRT,” Kavanagh told the symposium audience.2,3
SBRT applications may be integrated with emerging targeted-molecular chemotherapy agents for patients with genetic cancer predispositions, Kavanagh predicted. Preliminary data from a phase II clinical trial already suggests SBRT may improve survival rates achieved with erlotinib (Tarceva) in patients with non-small cell lung cancer (NSCLC) by as much as 12 months compared with survival rates of patients receiving erlotinib alone. (This study was not a randomized, controlled trial, however, and the comparison is based on a previous series of patients treated with erlotinib alone.)
Personalized therapies may represent major advances for patients with rare, genetic-vulnerability cancers. Kavanagh cited SBRT therapy with crizotinib, an experimental chemotherapy agent that blocks a molecular pathway involved in tumor growth in 5% of patients with NSCLC, for example. Crizotinib has very limited long-term efficacy because of the rapid evolution of crizotinib-resistant tumor clones, but patient survival times may be prolonged with SBRT.3 Kavanagh and his colleagues at the University of Colorado are using SBRT to target crizotinib-resistant tumors as they are detected, though a formal evaluation of this approach has not yet been completed.
Dheerendra Prasad, MD (medical director, Radiation Medicine, Roswell Park Cancer Institute, Buffalo, New York), argued that currently prevailing preferences for whole-brain irradiation over stereotactic brain radiotherapy for the treatment of intracranial metastatic tumors may be changing as the role of salvage therapy in prolonging patient survival times is increasingly appreciated.5
In clinical trials, superior tumor control and progression-free survival was superior for patients who received whole-brain radiotherapy combined with stereotactic radiosurgery compared with patients who received only stereotactic radiosurgery, Prasad acknowledged. However, those trials failed to account for salvage therapy following treatment failure.5 Metastatic brain cancer patients who received stereotactic radiosurgery first required fewer salvage treatments than patients who underwent whole-brain irradiation.5 Nor did previous clinical trials measure the impact of neurocognitive impairment on quality-of-life, Prasad said. Irradiating the entire brain can eradicate undetected microtumors; however, healthy brain tissue is also irradiated, impairing memory and fine motor control functions.5
SAFETY CONCERNS
As more aggressive radiotherapeutic regimens become widespread, identifying potential points of failure and ensuring radiation safety for patients and radiotherapy personnel becomes imperative, noted Eric Ford, assistant professor of Radiation Oncology and Molecular Radiation Sciences (Johns Hopkins University, Baltimore, Maryland). “Potential points of failure are scattered throughout the treatment process, so systematic tools must be developed that can uncover them when quality assurance does not,” Ford said.
Radiation therapy should borrow the failure mode and effects analysis techniques originally developed in the automotive and software industries, Ford argued.6 These tools allow analysis of the probability and severity of a potential failure based on historical data, including detailed data on near misses, and are a regulatory requirement for radiation therapy equipment manufacturers but not radiotherapy clinics.6
Pretreatment safety checklists such as those used by airline pilots (and in medical surgery, anesthesiology, and infection control) are powerful tools for ensuring safety but only if they are consistently and correctly used. For example, a simple five-item checklist has dramatically reduced the rate of opportunistic central-line catheter infections at Johns Hopkins, Ford reported.6
“It’s really about more than checklists,” Ford said. “It’s about standardization—figuring out the important tasks, how to do them, and doing them the same way every time.” Portal-dosimetric comparisons of planned and delivered radiation doses, and forcing functions as simple as using patient bar codes to confirm patient identities and treatment records, play a key role in radiotherapy safety. ONA
Bryant Furlow is a medical writer based in Albuquerque, New Mexico.
REFERENCES
1. Future of Radiation Medicine Report. Norcross, GA: Elekta; 2011. www.elekta.com/assets/Elekta-Oncology/pdfs/symposium/Future%20of%20Radiation%20Medicine%20Report-May.pdf. Accessed July 8, 2011.
2. Future of Radiation Medicine 2011 Clinical Leadership Symposium. www.elekta.com/healthcare_international_future_of_radiation_medicine.php?utm_source=future&utm_medium=redirect&utm_campaign=redirects. Accessed July 8, 2011.
3. Timmerman RD, Kavanagh BD. Advances in stereotactic body and image guided hypofractionated radiation therapy. Presented at: Future of Radiation Medicine Report; February 17, 2011; Scottsdale, AZ. www.elekta.com/assets/Elekta-Oncology/pdfs/symposium/Future%20of%20Radiation%20Medicine%20Report-May.pdf. Accessed July 8, 2011.
4. Timmerman R, Paulus R, Galvin J, et al. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA. 2010;303(11):1070-1076.
5. Prasad D. Brain metastases: stereotactic radiosurgery vs. whole brain radiation therapy. Presented at: Future of Radiation Medicine Report; February 17, 2011; Scottsdale, AZ. http://www.elekta.com/assets/Elekta-Oncology/pdfs/symposium/Future%20of%20Radiation%20Medicine%20Report-May.pdf. Accessed July 8, 2011.
6. Ford E. Radiation safety: identifying and improving points of potential failure. Presented at: Future of Radiation Medicine Report; February 17, 2011; Scottsdale, AZ. http://www.elekta.com/assets/Elekta-Oncology/pdfs/symposium/Future%20of%20Radiation%20Medicine%20Report-May.pdf. Accessed July 8, 2011.