Secondary cancers are widely recognized as possible outcomes of cancer therapy. However, radiotherapy and chemotherapy can also trigger life-threatening vascular accidents or initiate and hasten progression of cardiovascular disease, which increases the risk of vascular events in cancer survivors. New research highlights the importance of careful radiotherapy planning to avert avoidable sequelae in the coronary arteries of some cancer patients.
The risks of cardiovascular and cerebrovascular events (eg, thromboembolism, ischemia, heart attack, and stroke) appear elevated in cancer patients receiving certain treatments.1-4 Coronary artery thrombosis occurs up to 5 times more often in cancer patients with existing atherosclerotic disease receiving radiation therapy to the chest.1 Radiotherapy for Hodgkin disease and breast, lung, and head and neck tumors can initiate or accelerate atherosclerotic disease of the coronary and carotid arteries, posing a threat to patients’ lives decades after treatment is completed. Chemotherapy agents such as cisplatin, L-asparaginase (Elspar, Erwinaze), sorafenib (Nexavar), and bevacizumab (Avastin) can trigger cerebrovascular accidents.1
RISKS FOR BREAST CANCER PATIENTS
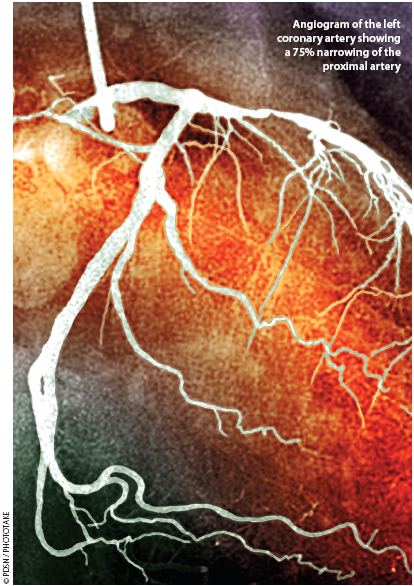
The heart is just below the chest wall, to the left side of the chest. Its valves, muscle, and vascular tissue are frequently irradiated during radiotherapy for a breast tumor. But a recently published Swedish study suggests the coronary arteries may be particularly vulnerable to radiation-associated stenosis.5 Vascular trauma can lead to progressive atherosclerotic plaque accumulations that occlude the arterial lumen, limiting local blood supply. The accumulation of plaque and scar tissue progressively occludes the lumen and impedes blood flow, contributing to ischemia. When plaque becomes dislodged and travels downstream to smaller-diameter vasculature, thromboembolytic events such as heart attack and stroke can occur.
This new research reports breast cancer patients receiving irradiation to the left breast, where more of the heart is exposed to ionizing radiation, were 700% more likely to develop high-grade (grade 4 or 5) coronary artery stenosis than were breast cancer patients who did not receive radiotherapy, compared with a 190% increased risk of stenosis with right-breast radiotherapy.5 The study reviewed cancer registry and coronary angiography registry data for 199 Swedish females with a breast cancer diagnosis between 1970 and 2003 and subsequent referral for coronary angiography between 1990 and 2004. It was the first study to specify the anatomic distribution of radiation-associated coronary artery disease.6 The authors identified the mid and distal left anterior descending artery, distal diagonal coronary artery, and the proximal right coronary artery as hotspots for breast cancer radiotherapy-associated stenosis.5 Left-breast irradiation was associated with a significantly greater risk of coronary artery stenosis than right-breast irradiation.5
“This makes perfect sense given the location of typical radiotherapy fields,” note radiation oncologists Timothy Zagar, MD, and Lawrence Marks, MD, of the University of North Carolina at Chapel Hill, in a commentary on the new study.6 “The study was carefully conducted, clever, and addresses an important clinical challenge. The results lend additional support to mounting evidence that radiotherapy can cause coronary artery disease and that there seems to be an association between the location of the radiotherapy beam and the location of the excess coronary events.”
“Radiation oncologists should exploit available tools (and) techniques to reduce doses to cardiovascular structures,” Zagar and Marks advise. Careful selection of gantry angles that spare the heart tissues and breath-hold maneuvers that increase physical separation between the breast and chest wall and heart are recommended. Conformal field shaping using a heart block also offers “an easy way to markedly reduce cardiac exposure when using left-sided tangents,” suggest Zagar and Marks.
CORONARY ANGIOGRAPHY REFERRALS MORE LIKELY AFTER RADIOTHERAPY
However, Zagar and Marks also suggest that radiotherapy patients were possibly more likely to be referred for coronary angiography than patients without a history of chest radiotherapy, a possible source of bias in the Swedish study.6 “Patients with potential cardiac symptoms and a previous history of radiotherapy might have been more likely to be sent for an angiogram than those who had not received previous [radiotherapy],” they noted. In this patient population, incidence of breast cancer was 10% higher for tumors in the left breast than for tumors in the right breast.5
 The Swedish study’s authors suggest regarding coronary arteries as at-risk radiosensitive tissues and advise making every effort to avoid radiation exposure to the coronary arteries.5 Contemporary low-risk conformal radiotherapy regimens lead to coronary artery stenosis less frequently than do less-focused irradiation, the authors said, highlighting the importance of planning and careful calibration and quality control programs for radiotherapy equipment.5 These risks should be explained to breast cancer patients, particularly those patients whose disease is in their left breast and who are contemplating lumpectomy with radiotherapy or mastectomy with no irradiation.5
The Swedish study’s authors suggest regarding coronary arteries as at-risk radiosensitive tissues and advise making every effort to avoid radiation exposure to the coronary arteries.5 Contemporary low-risk conformal radiotherapy regimens lead to coronary artery stenosis less frequently than do less-focused irradiation, the authors said, highlighting the importance of planning and careful calibration and quality control programs for radiotherapy equipment.5 These risks should be explained to breast cancer patients, particularly those patients whose disease is in their left breast and who are contemplating lumpectomy with radiotherapy or mastectomy with no irradiation.5
“Most radiation oncologists do not define the coronary arteries as structures to be avoided, but perhaps we should,” acknowledge Zagar and Marks.6 The Swedish study supports previous research linking breast cancer radiotherapy to coronary artery disease as well as other cardiovascular disorders including pericarditis, heart failure, heart valve disease, and even peripheral artery disease.6,7 However, the study encompasses a wide time period and includes patients treated with increasingly uncommon high-risk, unfocused radiotherapy treatments. In addition, latency periods for cardiovascular outcomes can be a decade or more for many patients, leaving the exact levels of risk posed by coronary artery irradiation unclear. Technological improvements have allowed more conformal radiotherapy that reduces the number of patients exposed to unfocused, high-risk therapy; however, for those patients who have received high-risk therapies, the risks of cardiovascular disease and cardiovascular-specific death may remain elevated throughout their lifespan. In a 2005 meta-analysis, radiotherapy after lumpectomy or mastectomy improved cancer-specific and overall survival rates.8 But the study identified a 27% overall increase in cardiovascular deaths among these patients, with no decline in risk evident 15 years after treatment.8
