Tungsten-alloy multileaf collimator (MLC) technology, borrowed from traditional external-beam radiotherapies, promises to reduce costs and delivery times for proton beam therapy, an emerging dose-escalated treatment for tumor control. But a new computer modeling study from the Indiana University Health Proton Therapy Center raises concerns about potential secondary and residual neutron radiation doses—particularly to staff—generated by tungsten’s interactions with proton fields. Oncology Nurse Advisor spoke with a senior author of that study and critics who say real-world proton therapy is much safer than the Indiana University study suggests.
PROTON BEAM RADIOTHERAPY
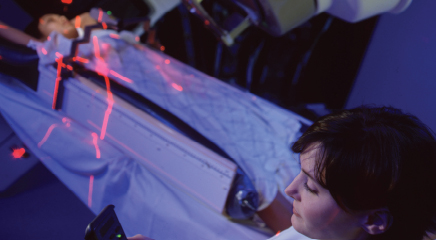
The tumor-killing radiation doses that can be delivered via traditional external-beam photon or gamma radiotherapy have long been limited by patient morbidity associated with the irradiation of healthy tissues. The promise of proton beam radiotherapy stems from protons’ dose distributions, which allow more precisely targeted, escalated-dose irradiation of tumor tissues while reducing doses to nontarget tissues. The large mass of charged particlelike protons reduces beam broadening and side scatter along beam pathways compared with that seen with other external-beam radiotherapies, for example. And along beam paths, protons’ Bragg peak distributions are very narrow, delivering very little radiation to skin at the beam-entrance site or tissues behind or below target tissue.1
 Those dose distributions offer an appealing alternative to other modalities, particularly, it has been argued, for children or young adults, for whom secondary cancers are a significant concern.1-3 But proton therapy facilities are expensive, with initial set-up costs of approximately $225 million.2 Patient-specific beam-shaping brass apertures used in proton therapy also drive up costs—up to $2,550 per aperture.3
Those dose distributions offer an appealing alternative to other modalities, particularly, it has been argued, for children or young adults, for whom secondary cancers are a significant concern.1-3 But proton therapy facilities are expensive, with initial set-up costs of approximately $225 million.2 Patient-specific beam-shaping brass apertures used in proton therapy also drive up costs—up to $2,550 per aperture.3
MULTILEAF COLLIMATORS SAVE TIME AND MONEY
An intuitively attractive cost-control measure for proton therapy has been to sidestep the use of expensive and labor-intensive brass apertures by modifying tungsten multileaf collimators (MLCs) already widely employed for intensity modulated radiation therapy (IMRT) and 3-dimensional conformal radiotherapy (3DCRT).3 MLCs allow a set of adjustable leafs to easily reshape radiation beams to patient-specific plans. Developed in the 1990s to replace cerrobend blocks, MLCs dramatically simplified IMRT radiotherapy workflows.
Unfortunately, proton beam interactions with field-modifying equipment (including MLCs, double-scattering systems, and range compensators) produce secondary neutron radiation exposures, raising concerns about potential secondary cancer risks.3-6 The long-term effects of secondary neutron radiation have been little-studied, and the risks of low-dose neutron irradiation remain poorly understood.7
SECONDARY AND RESIDUAL NEUTRON IRRADIATION
Now, a complex computer-modeling study published in the December 2011 issue of Medical Physics suggests the resulting ambient neutron radiation doses could reach 100 µSv per hour on the patient’s side of the proton beam collimator and 27 times higher than that upstream of MLCs. The team’s model predicts secondary neutron doses to patients to be at least 1.5 times higher when tungsten MLCs are used than will be the case with brass apertures, and the upstream ambient radiation dose to be 220 times higher for tungsten than brass.3
What’s more, the team found the buildup of residual neutron activity induced by proton fields is much steeper over time for tungsten than brass, requiring prolonged storage for activity cooling.3 That could become a significant occupational-exposure issue at centers with large patient populations, according to the study’s authors at Indiana University School of Medicine and the Indiana University Health Proton Therapy Center (formerly the Midwest Proton Radiotherapy Institute) in Bloomington.
Although based on a worst-case scenario of a fully closed tungsten MLC, these predicted doses could lead to an accumulated dose for radiotherapy staff that may exceed the occupational maximum permissible dose of 50 µSv/yr, the authors concluded.3 “The transfer of the tungsten MLC technology from megavoltage photon beams to proton therapy should be carefully examined in the context of secondary neutron yield from the collimator and associated secondary cancer risk,” the team reports.3 “Usage of tungsten MLC in [the proton beam therapy] clinic may create unnecessary risks associated with secondary neutrons and induced radioactivity for patients and staff, depending on patient load.”
Neutron dose associated with proton field irradiation of tungsten is not a new concern. Two 2009 studies suggested tungsten yields higher neutron doses than brass. One of these studies reported neutron doses to be higher with tungsten than apertures made of any other material studied—cerrobend, brass, iron, or nickel.8 The other 2009 study found a tungsten MLC to yield up to twice the neutron dose of brass collimators.9 (However, a third study published the same year found tungsten collimators in a double-scattering proton unit to reduce secondary neutron doses compared with those associated with brass.10)
There is “very little staff can do” about the predicted ambient neutron radiation dose, according to coauthor Indra J. Das, PhD, Director of Medical Physics for Indiana University’s Department of Radiation Oncology and the Indiana University Health Proton Therapy Center. “It is the poor selection of material,” Das told Oncology Nurse Advisor. “When designing MLC, one has to choose low atomic number materials.”