Diagnostic and therapeutic radiation have prolonged and improved millions of patients’ lives, and represent indispensable and increasingly sophisticated tools in clinical oncology. But medical radiation’s gifts have come at the potential cost of unintended irradiation of patients and health care workers and increased lifetime risks of secondary cancers. This concern has grown with improving patient survival times, particularly among pediatric cancer patients.
Occupational studies have been reassuring, suggesting rates of radiation-associated cancers are not higher in nurses with the possible exception of lung cancer, but this possible link is confounded by smoking behaviors.1 However, there is evidence that medical radiation may increase cancer risks among other health care workers and that those risks declined during the 20th century as a result of improved radiation safety practices.2
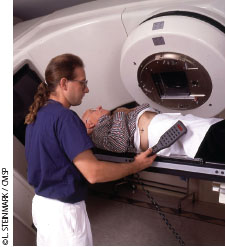
With increasing utilization of medical radiation, all health care workers should observe radiation safety practices to minimize risks to both patients and health care workers. Radiotherapeutic advances like intensity-modulated radiation therapy (IMRT), for example, allow escalated radiation dose delivery to tumors while minimizing irradiation of a patient’s healthy, nontarget tissue. However, these advances have come with increased risks when targeting errors occur, such as those caused by patient movement or improper patient setup. IMRT also requires complex three-dimensional (3-D) computed tomography (CT) planning examinations that may frequently involve unnecessarily high radiation doses. Combined with an upward trend in patient radiation doses over recent decades, and improved cancer patient survival times, such considerations raise troubling questions about medically unjustified radiation doses and secondary tumor risks.
TROUBLING REPORTS
The New York Times reported in 2009 and 2010 that serious brachytherapy dosing errors had occurred at the Veterans Affairs Medical Center in Philadelphia, Pennsylvania, and elsewhere.3 The journal Lancet Oncology had similarly warned in 2009 that staffing shortages and linear accelerator miscalibrations and quality control lapses had caused radiation dosing errors affecting thousands of cancer patients worldwide.4
 News reports led to renewed calls for interdisciplinary coordination; research; education; and effective, evidence-based policy-making and policy implementation to ensure radiation safety in radiation oncology and medical radiology in general.4-8 Unnecessary procedures, usually imaging procedures, and radiation dosing errors represent most of the risk for patients from medical radiation, whereas incidental, unintended radiation exposure is the primary concern for nurses and other health care workers.
News reports led to renewed calls for interdisciplinary coordination; research; education; and effective, evidence-based policy-making and policy implementation to ensure radiation safety in radiation oncology and medical radiology in general.4-8 Unnecessary procedures, usually imaging procedures, and radiation dosing errors represent most of the risk for patients from medical radiation, whereas incidental, unintended radiation exposure is the primary concern for nurses and other health care workers.
The American Society of Radiation Oncology (ASTRO) released an evidence-based white paper on quality assurance and safety for IMRT in 2011, the first of a planned series of expert-panel radiation oncology safety guidelines initiated after The New York Times‘ report.9 IMRT involves numerous hand-offs of patients and developing radiotherapy plans; ASTRO’s expert panel cautioned that radiation oncologists, physicists, radiation oncology nurses, radiation therapists, and dosimetrists should coordinate with one another to safely implement treatment plans, given the increased opportunities for miscommunication and error.9
CHALLENGES AND RESOLUTIONS
Interdisciplinary communication, quality control and assurance protocols, adequate radiotherapy staffing, and forced plan-review “time-outs” when ambiguities or concerns arise during radiation delivery are all crucial to avoiding catastrophic errors, the report concludes. Any member of a radiotherapy team should be empowered to call for a time-out or pause if concerns arise during radiotherapy procedures.9 Regardless of time pressures, a “no-fly” policy must be observed to prevent proceeding with treatment when errors in calculations, patient positioning and setup, or equipment settings are suspected. Written standard operating procedures should be on hand at every radiotherapy facility, for each radiotherapeutic procedure conducted.9 Time pressures, exacerbated by inadequate staffing, can lead to skipped quality-assurance checks and dosing errors.9 Simple checklists are essential when implementing complex radiotherapy treatment plans.9
Incorrect dose calculations, incorrect patient setup, incorrect beam intensity calibration, and equipment or software failures are leading factors in radiotherapy dosing errors.10 Insufficient training for a particular radiotherapy procedure, distraction or inattention to detail, a failure to conduct independent beam calibration checks before treatment, and the absence of clear written procedures are all prominent factors underlying dose errors.10 Most problems can be avoided by diligent compliance with quality-assurance and control procedures, including double- checking calculations, treatment plans, and equipment settings and regular equipment calibration checks.9 However, these hinge importantly on adequate staffing.9
Minimizing radiation exposure to medically justified levels begins even before the patient arrives at the radiotherapy department. The appropriateness of radiotherapy should be carefully considered. Inappropriate prescribing of radiotherapy can result from physician error, habit, patient preference, or even reimbursement incentives. For example, some urology clinics that own IMRT equipment may prescribe IMRT for elderly patients with prostate cancer when watchful waiting would be more appropriate.11
The diligent use of protective shielding, careful positioning of health care workers away from scatter radiation during patient irradiation, and use of thermoluminescent dosimeters (TLDs) or other personal radiation-dosimetry equipment are fundamental radiation-safety practices. A facility-level culture of safety requires attention to detail, patience, avoidance of shortcuts, annual equipment checks and calibrations, independent reviews of treatment plans, and review of calculations and equipment settings.10
