The clinicopathologic and genetic features of marginal zone lymphomas (MZL) with histologic transformation (HT-MZL) suggest that they may be a distinct tumor type from other MZLs. In addition, the higher rates of TBL1XR1 mutations in HT-MZL suggest this could be a predictor for transformation.
The study, which was published in the journal Cancer, analyzed the clinicopathologic features and genetic alterations of 535 patients with MZL, 174 cases of de novo diffuse large B-cell lymphoma (DLBCL), and 43 HT-MZL. Genetic analysis included a 148-gene targeted exome sequencing assay.
Baseline characteristics between patients with MZL and HT-MZL were similar, except higher rates of bone marrow involvement (P =.0041) and higher levels of lactate dehydrogenase (P =.0001) were present with HT-MZL. In both types, the median age at diagnosis was 60 and the most common sites of disease were lymph nodes and the stomach.
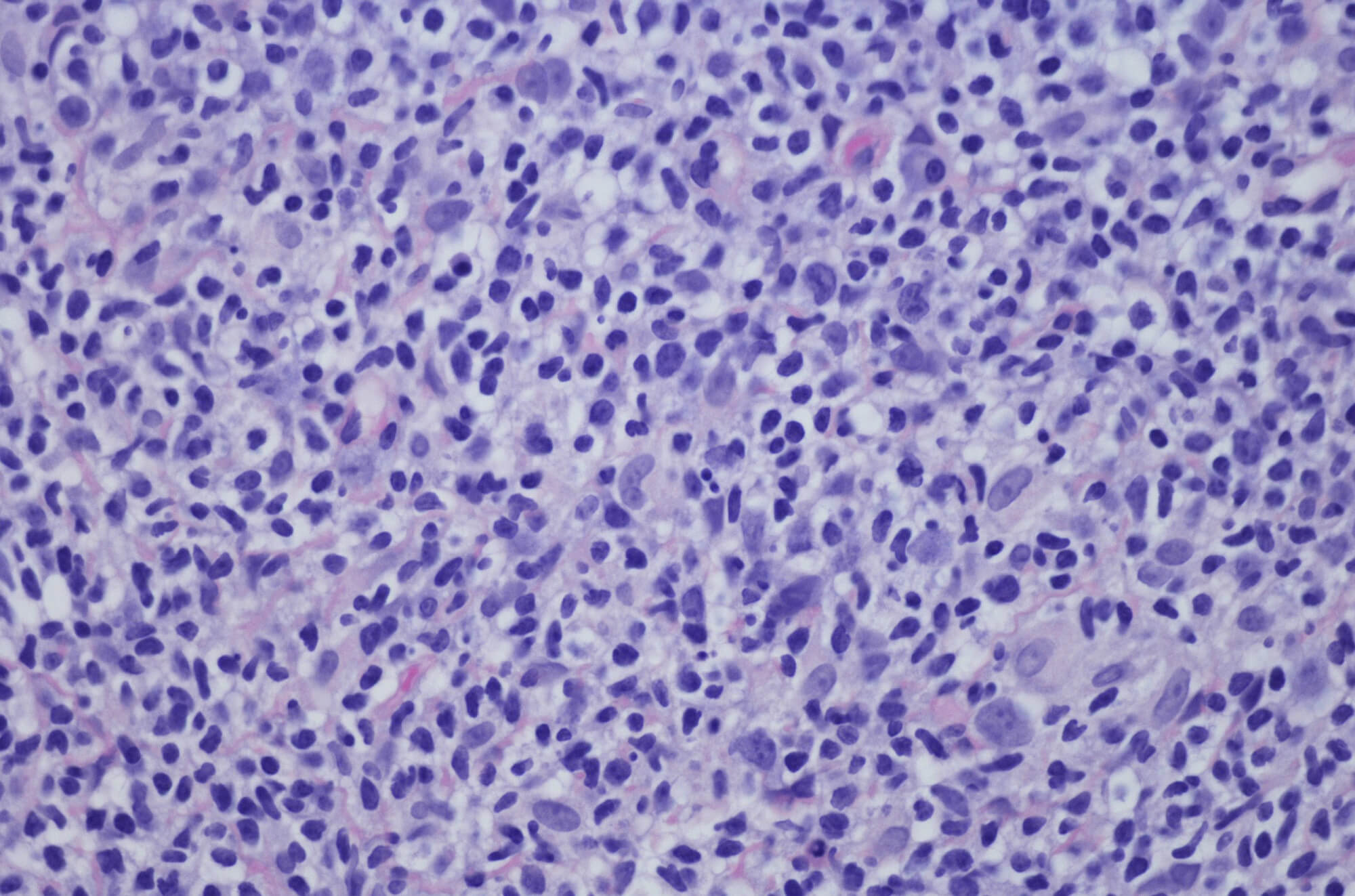
All HT-MZL cases corresponded to DLBCL, either through diagnosis of DLBCL with an MZL component or history of MZL. The median time to histologic transformation was 19 months.
The most commonly mutated gene in HT-MZL was TBL1XR1, which was present in 63.6% of cases, compared with 7.7% in MZL (P =.0001) and 26.4% in non-GCB-type DLBCLs (P =.009). Other commonly mutated genes included CCND3 in 31.8% of cases and CARD11, ID3, and TP53, which were each mutated in 22.7% of cases.
The frequency of TLB1XR1 and ID3 mutations were significantly higher among patients with HT-MZL compared with patients with MZL or non-germinal center B-cell type DLBCLs.
HT-MZL cases were also more likely to have upregulation of BCL6 (P <.0001), MUM1 (P =.001), C-MYC (P <.0001), and Ki-67 (P <.0001) compared with MZLs. Recommended cut-off values for expression of BCL6, MUM1, C-MYC, and Ki-67 were 2.5%, 2.5%, 7.5%, and 23.5%, respectively, for transformation, as indicated by receiver operator characteristic curve analysis. There were no MYC, BCL2, or BCL6 rearrangements detected among patients with HT-MZL.
“Our study demonstrates, that compared with MZLs, HT-MZLs display a distinct immunophenotype,” the authors concluded in their report. “Despite the similar immunophenotype, the mutation profile of HT-MZLs…differs from that of non-GCB-type DLBCLs, suggesting a distinct evolutionary process.”
Reference
Li A, Yi H, Deng S, et al. The genetic landscape of histologically transformed marginal zone lymphomas. Cancer. Published online November 8, 2023. doi:10.1002/cncr.35072
This article originally appeared on Hematology Advisor