Standardizing care and improving interdisciplinary communication rapidly improves quality of care for patients undergoing radiation therapy for head and neck cancers (HNC), according to Maura Kenny, RN, BSN, OCN, a radiation oncology nurse at the Hartford Healthcare Cancer Institute in Hartford, Connecticut. Her team’s findings were presented at the 48th Annual Oncology Nursing Society (ONS) Congress.
Nearly 4% of all cancers diagnosed in the United States are HNC and most (approximately three-quarters) are associated with HPV; tobacco and alcohol use are other key risk factors. Seventy patients a year undergo radiation therapy for HNC at the Institute’s Helen & Harry Gray Cancer Center, Kenny noted.
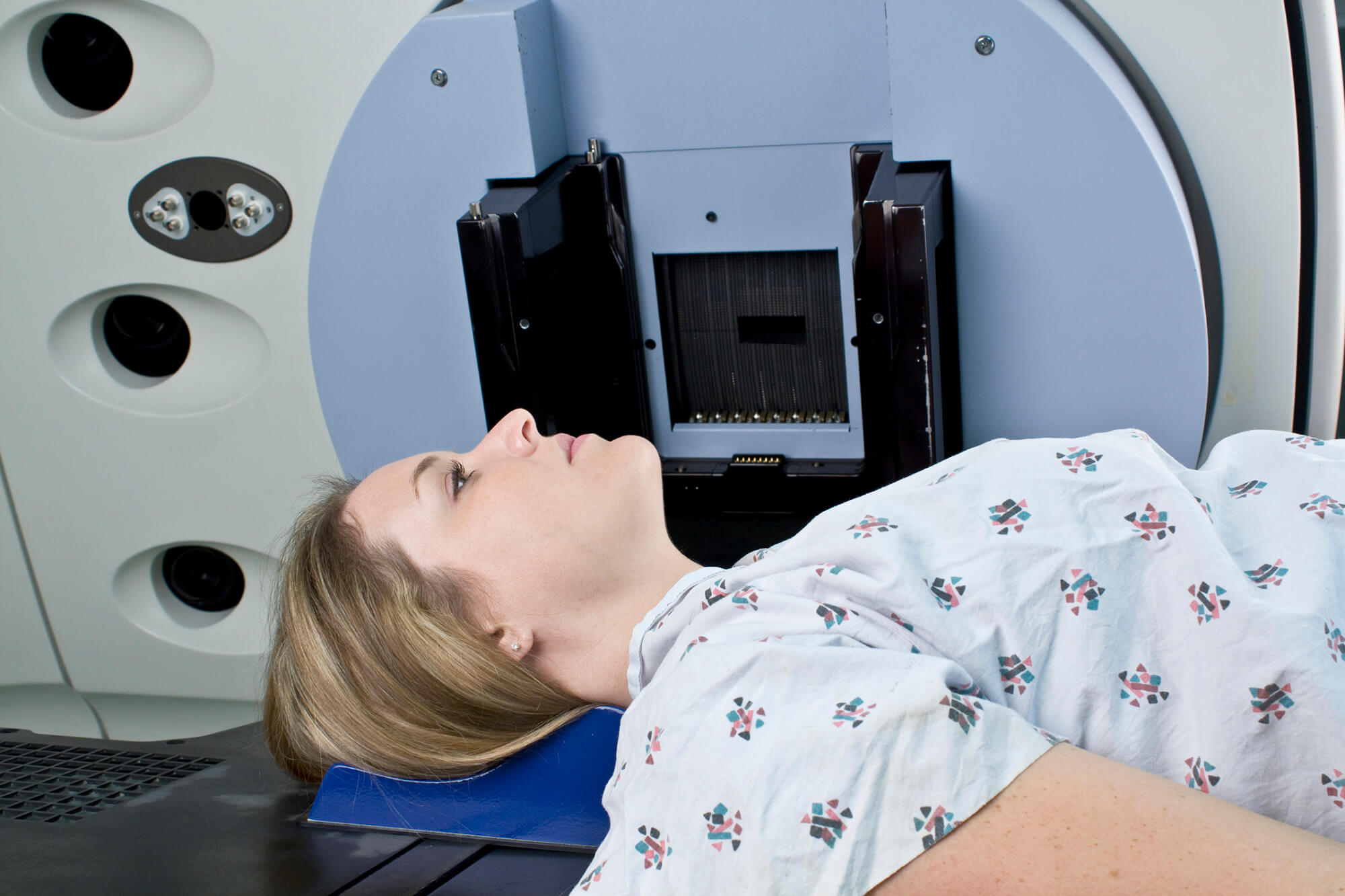
Patients undergoing radiotherapy for HNC frequently present with multiple comorbidities and go on to experience significant radiation toxicities, leading to treatment interruptions, hospitalizations, and declining health and quality of life, Kenny said. Nearly all will develop oral mucositis, a painful and debilitating radiotoxicity.
“Data suggests that improved communication and standardization can reduce these adverse events,” she said. To improve care standardization and communication between clinicians in inpatient and outpatient settings, the center started providing new patients with a kit and instructions for a baking soda/salt (BSNa) oral mucositis mouth rinse, and collecting “qualitative data” (documenting descriptive observations) in weekly multidisciplinary HNC patient rounds involving the radiation nurse and a social worker, a speech therapist, and a dietician.
Care was also standardized for inpatients undergoing radiotherapy with an HNC order set that includes Ensure Enlive (8 oz) nutritional supplements 3 times a day between meals, daily body weight measurements, nurse reminders for oral care (after meals and nightly, with a soft toothbrush; rinse, gargle, and spit with mouth rinse every 2 hours), triamcinolone 0.1% cream typically applied twice daily, nutritional services consultation, and speech therapist evaluations and treatment, including clinical bedside swallow evaluation and treatment.
Multidisciplinary rounds identified 1 to 2 patients each week who were missing social worker referrals, and 5 patients requiring prioritized assessments for weight loss, Kelly reported.
“First day packets have qualitatively improved performance of BSNa rinses, particularly among underserved/under-resourced patients historically at risk for adverse outcomes,” Kelly said.
Improved standardization of care and communication across disciplines and care settings for patients with HNC are possible, and has produced rapid qualitative improvement in patient care, she concluded.
Reference
Kenny M, Marcelino N. Bridging gaps & standardizing care among head & neck cancer patients receiving radiation. Oral presentation at: 48th Annual ONS Congress; April 26-30, 2023; San Antonio, Texas.