The human body is far more complex than the sterile arrangements of genetically identical, specialized, and cooperating human cells suggested by textbook anatomy and physiology schematics. It is a byzantine, interacting ecosystem of diverse, thriving communities of bacteria, fungi, protozoans, and viruses. The human genome even includes “fossil” endogenous retroviruses — genes from ancestral infections incorporated long ago into our species’ genetic inheritance.1
The living nonhuman components of our bodies’ ecosystems are called the microbiome, sometimes described as humanity’s “second genome.” The emerging field of metagenomics seeks to sequence microbial DNA alongside patients’ human genomes simultaneously.2
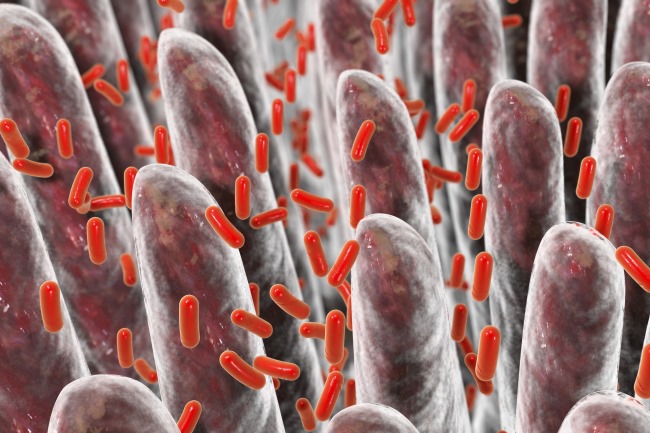
In reality, though, each of us contains numerous distinct microbiomes because these microbial ecosystems vary dramatically between different organ systems. They play essential roles in intestinal mucus layer composition, permeability, and repair; food digestion and nutrient absorption; immune system behavior; and resistance or proneness to disease.2-6
The species compositions of microbiomes and patient biology are linked in tremendously complex ways. Circadian sleep/wake cycles appear to affect gut bacterial communities, for example.7 Gut bacteria also release neuropeptides into patients’ bloodstreams that might affect appetite and mood.8,9
Microbiome oncology is a young field of study. Researchers are identifying myriad associations between microbiomes and individual microbial species, cancer, and cancer treatment. So far, relatively little is known about most of those associations’ underlying, causal molecular mechanisms.2 But researchers are already exploring whether the microbiome helps explain associations between tobacco smoking or diet, with cancer risk. (The bacterial makeup of pretreatment oropharyngeal microbiomes differs between smokers and nonsmokers.4)
Invasions by pathogenic microbes, or other microbiome disruptions — collectively called dysbiosis — are associated with metabolic disorders, autoimmune conditions, and cancers.3,10 There is evidence that some microbiomes are associated with reduced cancer risk, whereas dysbiosis and specific microbial species can be carcinogenic.2
Dysbiosis facilitates tumor formation, progression, and metastasis; immune system responses to tumor cells; and tumor responses to different cancer treatment modalities, including chemotherapy, radiation, and immunotherapy.11,12 (Distinct from host microbiomes in the tumor microenvironment, the microbiomes inside of tumors, or intratumoral microbiomes, have received less study but can reasonably be expected to be similarly important in understanding tumor behavior and treatment responses.13)
Microbiomes of the oropharynx, gastrointestinal tract, gut epithelia, urinary tract, and breast tissues are important components of tumor microenvironments; they can disrupt communication between tumor cells and affect host and tumor cell production of inflammatory cytokines, or they can facilitate tumorigenesis, progression, and treatment response in head and neck, colon, stomach, breast, and prostate tumors.3 Less is known about the lung microbiome or its roles in lung cancer.14
Gastrointestinal microbiomes’ connections to cancer are among the most studied. For example, there are well-established roles of the bacteria Helicobacter pylori in peptic ulcers, gastric cancers, and mucosa-associated lymphoid tissue (MALT) lymphomas.2 Fusobacterium may also facilitate tumorigenesis.15
Other bacteria appear to slow tumor growth or mitigate treatment side effects. Lactobacillus and Bifodacterium, for example, appear to increase cancer cell apoptosis (“cell suicide”) and to protect DNA from oxidative damage.7,15 Bifodacterium can inhibit tumor cell growth factors and block inflammatory cytokines in ways that might help explain its association with lower risks of adverse treatment effects such as radiation-associated gastrointestinal mucositis and diarrhea, or ipilimumab-associated colitis.7,15
Scientists are already investigating whether managing patients’ gut microbiomes through dietary modifications, probiotics, fecal transplantation between patients, — and even the targeted delivery of anticancer bacteria into tumor tissue or the use of tumor-seeking bacteria to deliver anticancer drug payloads — might offer new adjuvant components of cancer treatment, enhancing treatment efficacy and reducing toxicities.4,16
Microbiome and metagenomics research for chemotherapy and cancer immunotherapy are further along than studies of radiotherapy, but it does appear that microbes can impact radiotherapy and chemoradiotherapy, as well.7