Pencil Beam Scanning (PBS)
PBS offers a dosimetric advantage over double scattering technique with regard to conformality around OARs, particularly for irregularly shaped targets. PBS is useful when the target volume varies markedly in depth, and also when the target spans over a large field size. Consequently, PBS solves many of the treatment planning complications of DS by allowing irregular and non-contiguous targets with homogeneous target coverage and improved sparing of OARs. PBS allows for delivery of 3D conformal treatments with 1 to 2 fields without the need for multiple custom-built compensators and apertures, which can be a laborious procedure.
PBS field sizes tend to be larger than DS field sizes, thus larger targets can be easily planned. As noted above, if requiring treatment to a large target with DS, matched fields must be created (with separate apertures and compensators), which can often result in hot or cold dosimetric areas. Additionally, the “beam-on” time for PBS is often longer than for DS technique, making it more difficult to administer a DIBH method (if available). Also, there is more skin sparing with PBS compared to DS, and thus, overlapping beams on the skin are not a major concern. For example, PBS is able to shape the proton beam to conform to the shallow and deep aspects of the target, thus allowing for a “skin-sparing” effect. In DS system, the proton beam can only be shaped to conform to the deeper shape of the target, thus precluding a skin sparing effect for superficial targets. PBS beams are usually angled away from each other to allow for improved robustness. It is also important to note that the above-described margins for both techniques do not protect against unpredictable, uncommon changes that may occur during the course of treatment such as disease progression, pleural effusions, pneumonia (or pulmonary consolidation), or weight loss.
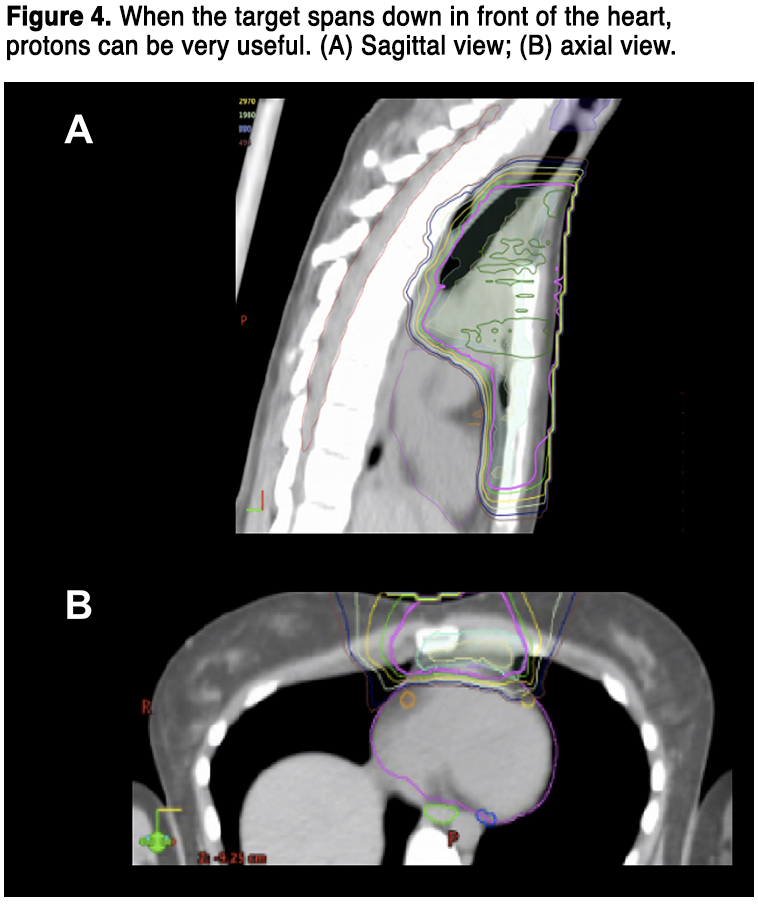
Overall, all of the available PT techniques are used to maximize cure and minimize the morbidity of treatment, and providers are encouraged to follow the current ILROG guidelines for proton beam therapy in adult radiotherapy programs.16 For this reason, a plan comparison between PT and a modern photon solution is strongly recommended before treatment, in order to demonstrate the beneficial role of protons. Indeed, it should be noted that the potential clinical benefit of PT over photon RT is greatly influenced by the disease extension and localization. As an example, some anatomical presentations as the lower anterior mediastinum mostly benefit from a PT solution. It is likely that if one encounters a case such as in Figure 4, in a young patient with curable disease, PT would be of significant dosimetric and clinical benefit.
CLINICAL REPORTS OF PROTON THERAPY FOR LYMPHOMAS
Modern radiotherapy for lymphomas combines smaller fields (involved site radiotherapy, ISRT, and involved node radiotherapy, INRT), lower doses and highly conformal techniques compared to the past. Given the higher conformal dose distribution achieved with protons, many investigators have raised the issue of the potential increased relapse rate, in particular at the field edge.
First, clinical reports were therefore focused on this question, as the main scope was to demonstrate the ability of PT to obtain the same cure rates of modern photon techniques. With this background, University of Florida conducted a phase II pilot study on 15 stage I–III HL patients, treated with involved-node PT between 2009 and 2013.21 With a median follow-up of 37 months, the 3-year relapse-free survival (RFS) rate was 93%, absolutely similar to the outcome obtained with modern photon radiotherapy in HL. Some clinical reports were subsequently published, with most of them focusing on HL patients with mediastinal involvement. The Proton Collaborative Group Registry reported on a cohort of 50 patients treated with consolidation proton ISRT and followed-up prospectively (median follow-up time: 21 months).22 Most patients were adults (64%), with a high prevalence of mediastinal involvement (93%) and of bulky lesions (65%). The overall outcome was good, with a 2-year RFS of 85%. There were only 3 relapses: two were infield, within bulky mediastinal lesions treated with 21 Gy, and one was marginal, superior to the treatment field and to the clinical target volume and for such reason would have been missed with a photon plan as well. Very recently, a collaborative group first reported the clinical results of a cohort of 21 adult HL patients treated with deep inspiration breath-hold PBS-PT.23 All patients were treated at 30 Gy in 15 fractions. With a median follow-up time of 24 months, no patient relapsed and all were alive. Treatment was well tolerated and no severe toxicities were reported.
Although most studies enrolled HL patients, few reports on small series of NHL patients are available. University of Florida first described their outcome with PT in a group of 11 NHLs, which included patients affected with a variety of different histologies.24 Three-year PFS and OS were 91%, with only one case of in-field relapse in a patient treated for a natural killer/T cell lymphoma. No severe toxicities (Grade >2) were reported. Afterward, Plastaras et al25 reported their experience with PT in a cohort of nodal NHLs with mediastinal involvement or primary mediastinal B cell lymphomas. Overall, 24 patients were enrolled, with a high predominance of bulky lesions at baseline (87%). The median follow up was 28 months and 2-year PFS and OS were 87% and 96%, respectively. Only one patient relapsed in-field and none had grade 2 or higher radiation pneumonitis. A recent publication from a German group26 enrolled 20 patients affected with either HL (9) or NHL (11). The outcome was, again, impressive with a 2-year PFS and OS of 95% and 100%, respectively. The toxicity profile was good as well, with a good tolerance to PT and no events of grade 3 or higher.
The adoption of PT is even more promising in the setting of relapsed/refractory disease, when peri-transplant radiation is frequently omitted despite its valuable effect for the concerns related to toxicity – mainly grade 2–3 pneumonitis – after photon RT. Tseng et al27 enrolled in a multi-institutional study 51 patients treated with PT for a relapsed/refractory HL or NHL. All patients were heavily pretreated and one third received peri-transplant PT. With a median PT dose of 36 Gy (range 25.2–54 Gy) and a median follow-up of 21 months, the 2-year progression-free survival (PFS) and overall survival (OS) were 69% and 87%, respectively. Obviously, HL patients had a better outcome compared to NHL patients in terms of both PFS (78% vs 46%) and OS (88% vs 82%). Only 6 patients (12%) developed a symptomatic grade 2 pneumonitis (no grade 3> toxicity event reported), which is lower compared to historical controls treated with photon RT. These preliminary results, that need to be confirmed in larger cohorts, seem to favor PT over photon RT in this setting, given the more conformal dose distribution of protons and ability to better spare fundamental organs at risk as lungs and heart.
Despite the brilliant clinical results, all the studies mentioned above included a small number of patients, mostly within a mono-institutional accrual, and thus a careful extrapolation is mandatory. To date, the largest multi-institutional case series of lymphoma patients treated with PT was published by Hoppe et al28 in 2017. The authors included 138 pediatric and adult HL patients. With a median follow-up of 32 months, the 3-year RFS rate was 92% for all (96% for adults, 87% for pediatric patients), with none marginal relapse. The accompanying editorial for this study29 celebrated the excellent clinical results, similar to those obtained with modern photon radiotherapy in HL. Interestingly, there were no marginal relapses potentially related to the rapid dose fall-off of the Bragg peak. This observation was extremely important, given that the combination of steep dose-gradient techniques with the modern definition of limited target volumes (INRT and ISRT) raises many concerns on the potential increase of relapses. More studies with similar or possibly larger numbers are mandatory to strengthen these preliminary observations and to increase the robustness of the information on the role of PT in lymphoma patients. Table 1 summarizes all clinical studies investigating the role of PT in this setting.
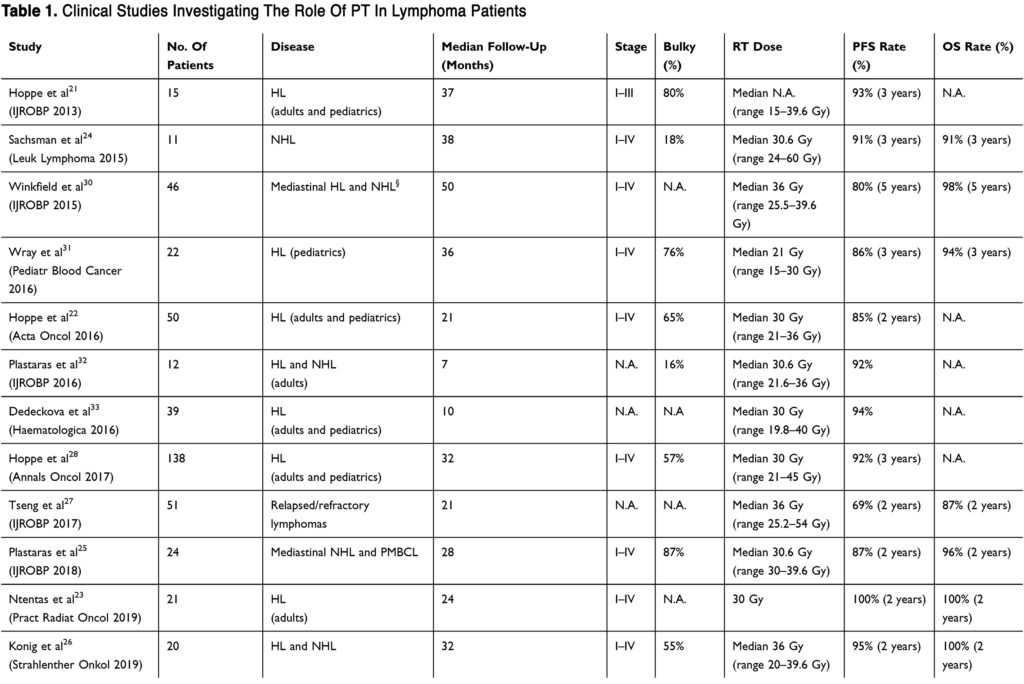
(To view a larger version of Table 1, click here.)
READ FULL ARTICLE
![]() From Dovepress
From Dovepress