UNCERTAINTIES OF PROTON THERAPY
The most relevant challenges associated with PT, compared to photons, are the uncertainties related to the different beam penetration range in tissues and to the changes in the magnitude of the relative biological effect (RBE) along the beam path.16 Herein below, we briefly describe these uncertainties and the possible ways to mitigate them.
Relative Biologic Effectiveness (RBE)
RT prescription and constraints are based on dose parameters and dose–response relationships, which are basically derived by photon therapy. Different radiation modalities may produce different dose responses, and this aspect is relevant also in the comparison between photon (the reference radiation by definition) and protons. This discrepancy is evaluated through the relative biological effect (RBE), which is the ratio of the absorbed dose that produces the same biological effect between photons and protons.34 The currently used RBE in clinical practice is 1.1, but some studies have demonstrated that this parameter depends on many factors as proton energy, dose per fraction, tissue and cell type, oxygenation and other aspects that may influence the radiosensitivity of the tissue.35,36 Moreover, RBE estimation of protons is derived by in vitro studies, but in vivo studies are still missing.37 Furthermore, actual data suggest that RBE may change along the beam path, with a significant increase at the beam tail in the proximity of the Bragg peak. This aspect is related to the increase of the linear energy transfer (LET) of the proton beam at the distal edge and raises many concerns on the estimation of the dose received by the target of treatment and, particularly, by organs at risk located in its close proximity. In fact, the increase in RBE at the beam tail may extend the beam range by 2–4 mm, depending on the depth in the target tissue and on the beam energy.38 This leads to a potential extension of the high-dose region beyond the target volume and may end up in organs at risk located behind the tumor.39 Paradoxically, this aspect may lead to the creation of hotspots in those structures that should be better spared with protons (i.e. heart and breasts) when treating mediastinal lymphomas. Given that RBE-based or LET-based planning is not available to date, precautions should be adopted to protect healthy tissues as the use of multiple fields to dilute the effect, or reduction of the physical dose to organs at risk located in the proximity of the distal edge.16
Uncertainties Due To Density Variations And Organ Motion
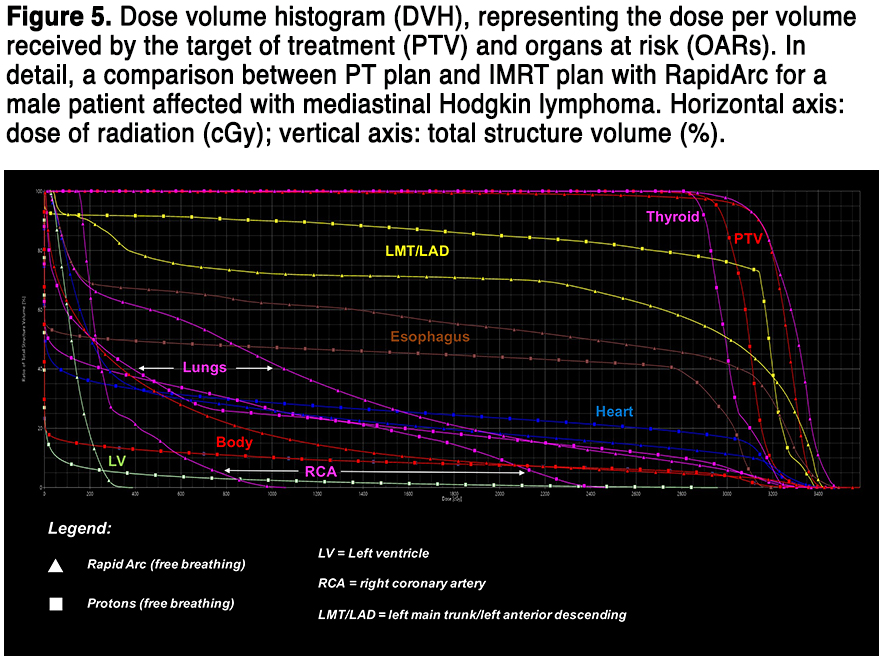
Protons are particle therapies with mass and, therefore, density of the tissues and organs encountered by the beam path greatly influences the dose deposited. Any anatomic variation in term of position and size – of both patient and tumor – could affect the dose distribution. Particularly, the axial deviations may translate in range uncertainties; in fact, the range of PT is related to every single voxel of the planning imaging and any minimal change of the patient anatomy (and consequently of the mass density and of the related voxel) will modify the range of all protons crossing that/those specific voxel.16,37 Strategies to mitigate this dosimetric uncertainty are strongly recommended, through the adoption of tracking techniques40 or a 4-dimensional CT scan to compensate for organ motion (mainly lungs).41 Moreover, large margins should be applied to account for the uncertainties due to the inevitable differences in tissue across the proton track. A compensatory margin could be considered also to “protect” very small and critical OARs as the coronary arteries, whose physiologic movement during the cardiac cycle is unavoidable.42 When the sparing of critical organs is mandatory, all these issues should be kept in mind and a comparative planning would be strongly recommended not only between different PT plans, but also with modern and highly conformed photon solutions as intensity-modulated RT (IMRT) and optimized volumetric arc therapy solutions.43 Indeed, in some particular anatomical situations (even in some patients with mediastinal involvement), the gradual fall of the dose around the target volume may favor IMRT, given the high risk of a “full-dose” extension to the organs at risk with PT for all the issues mentioned above.39 Therefore, patient selection is fundamental to estimate who might benefit mostly from the offer of a PT plan. A well-balanced planning comparison with a modern and optimized photon RT solution29 is thus mandatory, taking in to account PTV coverage and doses received by organs at risk. Figure 5 shows a dose-volume histogram, comparing a photon and a proton solution.
“IN SILICO” COMPARISON OF THE RADIATION LATE EFFECTS BETWEEN PT AND MODERN PHOTON RT
In a current radiation treatment, the difference between modern delivery techniques is characterized by a difference in the spatial distribution of radiation dose. Therefore, in lymphoma, there is a large variation in the normal tissue exposure among patients who nominally receive the same form of radiotherapy due to the individual differences in field size as well as in anatomical site of disease. Also, late effects most often occur decades following treatment and the excess risks reported in the literature are consequences of now outdated treatment regimens and should not be extrapolated to patients of today. Instead, the choice of an optimal treatment strategy can be guided by comparative dose planning and modeling studies.
Fourteen studies have evaluated the difference in organ at risk (OAR) exposure with involved node/site PT versus photon therapy in lymphoma (Table 2 for an overview). The studies compare PT delivered with either passive scatter (6 studies) or pencil beam scanning (7 studies) techniques to modern radiotherapy photon planning using 3-dimensional conformal RT (3DCRT, 12 studies) with anteroposterior-posteroanterior fields as well as to more conformal photon planning with IMRT (7 studies), volumetric modulated arc therapy (VMAT, 5 studies), or Helical Tomotherapy (2 studies). Three recent studies44–46 have also compared the benefits of deep inspiration breath-hold (DIBH) in different combinations with PT and IMRT.
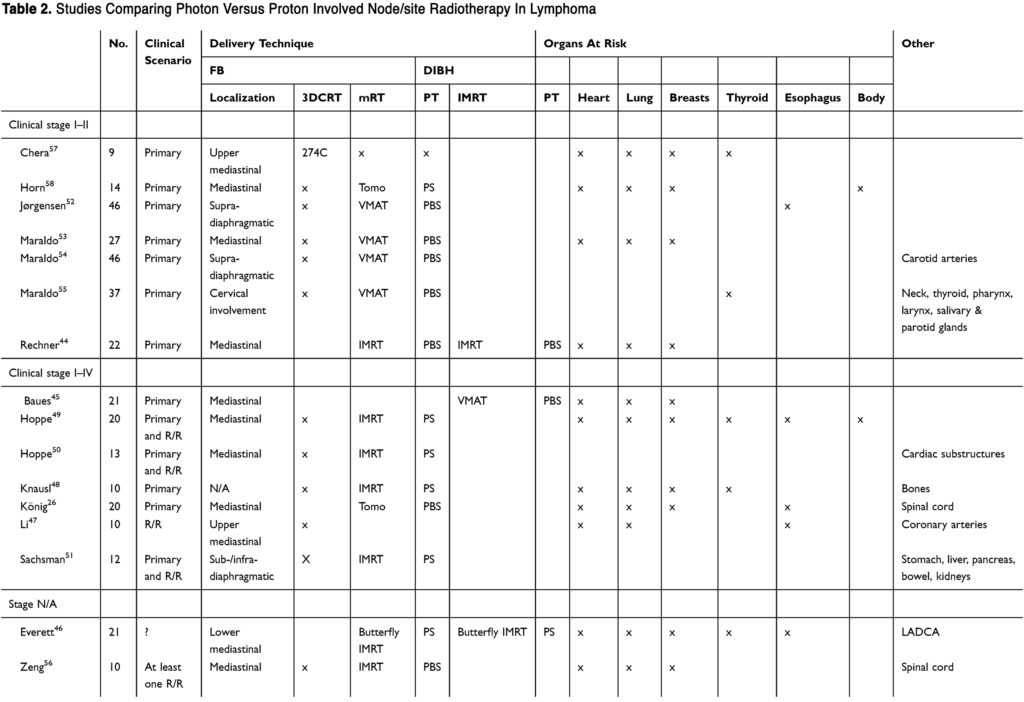
(To view a larger version of Table 2, click here.)
Importantly, several aspects should be carefully considered in the individual publications: 1) The patient population: what are the no. of patients, HL vs NHL histology, children vs adults, clinical stage, and primary vs relapsed/refractory disease, 2) Where is the target localized and how it is defined? Upper vs lower mediastinal presentation and initial vs residual post-chemotherapy disease, 3) Is information provided on photon planning field set-up, optimization priorities and plan evaluation? and 4) Do the authors have any proton planning experience? Is robustness and dose and range uncertainties accounted for? Among the 14 studies, three include HL and non-HL patients,26,46,47 one report only on pediatric patients,48 three include both primary and relapsed/refractory patients,49–51 five origin from centers without proton facilities,45,52–55 and two provide very limited clinical information.46,56 Also, two studies define the target volume as residual disease following chemotherapy47,57 and cannot be said to adhere to the INRT/ISRT concept. A summary of estimated doses to thoracic OARs in mediastinal lymphoma is provided in Table 3; however, due to the caveats mentioned above, considerable uncertainties apply for the reported absolute values.
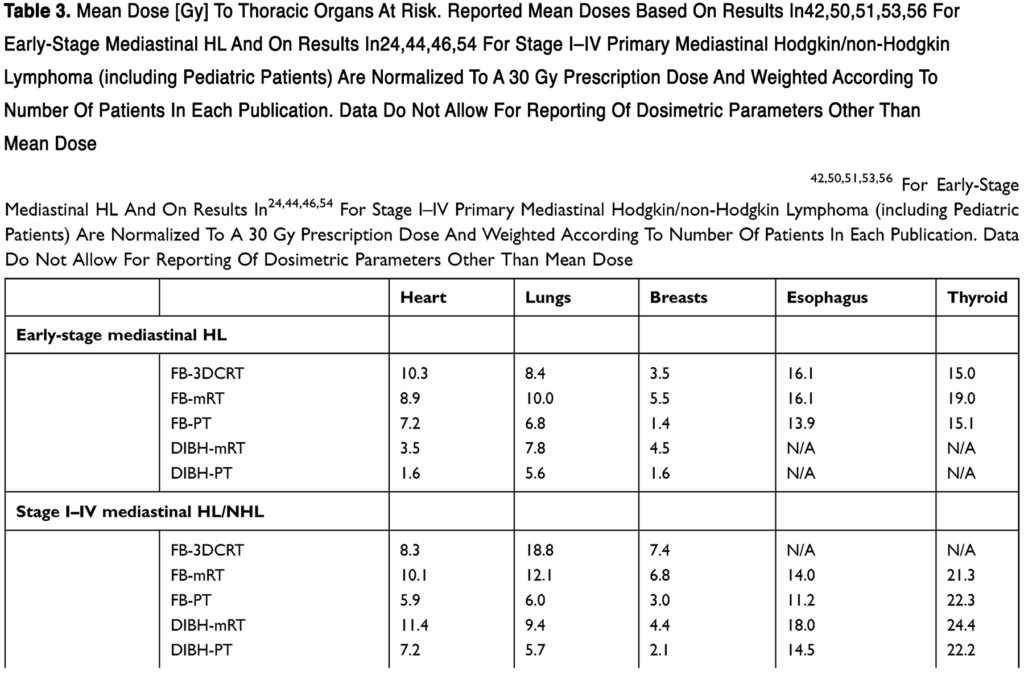
The following sections focus on primary mediastinal stage I–II HL where data are most robust. In free-breathing (FB), the mean doses to the heart, lungs and female breasts are estimated to decrease with PT compared to 3DCRT and modern RT (mRT). Interestingly, with DIBH-mRT, the estimated mean dose to the heart is even lower, almost similar for the lungs, and higher for female breasts which may be due to the low dose bath associated with rotational therapy and/or that most comparative dose planning studies in PT prioritize the female breasts the highest during planning. When PT is combined with DIBH, a further dose reduction may be achieved, especially for the mean dose to the heart, compared to FB-PT and DIBH-mRT. It is important to mention that this comparison cannot consider the differences in the high- and low-dose distributions between the individual studies which are equally important when choosing the optimal treatment plan. Also, all studies report large individual differences in dose estimates, and the importance of individualized treatment planning is highlighted universally.
The risk of late effects from modern treatment can be estimated through normal tissue complication probability (NTCP) models which describe the probability of a certain endpoint occurring as a function of radiation dose. For INRT/ISRT, only one NTCP study has been published,44 although, Knäusl et al48 calculate the organ equivalent dose which is as a measure of the biological effect of absorbed dose in pediatric patients. However, many photon-based NTCP models have been published to date for lymphoma patients.43,53,59–63 which can be extrapolated to calculate the clinical significance of a dosimetric benefit with PT. In the single PT-based modeling study available to date,44 the estimated reduction in life expectancy attributable to late effects from RT (from heart failure, myocardial infarction, valvular heart disease, lung and breast cancer) is quantified by the Life Years Lost (LYL) measure which accounts for age at exposure, patient sex, and the prognosis of the individual late effects. The authors report a LYL of 2.1, 1.3, 0.9, and 0.7 with FB-mRT, FB-PT, DIBH-mRT, and DIBH-PT, respectively, and the LYL is primarily driven by the risk of death from lung cancer and valvular disease. Interestingly, there is no significant difference in the LYL for FB-PT vs DIBH-mRT and FB-PT vs DIBH-PT, respectively. Again, modeling studies are limited by the same uncertainties as are dose planning studies as well as by the inherent simplifications of the modeling situation.
READ FULL ARTICLE
![]() From Dovepress
From Dovepress